Translate this page into:
Neutrophil-lymphocyte ratio among preeclampsia patients in India – A systematic review and meta-analysis

-
Received: ,
Accepted: ,
How to cite this article: Velusami D, Soundariya K, Mohan R, Mary JF, Ganapathy K, Sanjay P. Neutrophil-lymphocyte ratio among preeclampsia patients in India – A systematic review and meta-analysis. Glob J Health Sci Res 2023;1:63-8.
Abstract
Preeclampsia is one of the major causes of morbidity and mortality in pregnant females in India. Early detection of preeclampsia can be of clinical utility. Neutrophil Lymphocyte Ratio (NLR) is a simple hepatological biomarker that has been used for diagnosis of preeclampsia. With this perspective in mind, the present meta-analysis was planned to evaluate NLR among preeclampsia in the Indian setting. Databases systematically searched were PubMed, MEDLINE, and Google Scholar were systematically searched till July 2023. The studies selected were all Indian published articles NLR evaluated in females of age ≥18 years and < 40 years with preeclampsia and normal health pregnant females. Data extraction was guided by a predetermined checklist. Using RevMan 5 software, the mean and standard deviation were evaluated and analyzed. The initial search yielded 103 records of which 54 articles underwent evaluation, which identified 8 articles and a total 1381 study population. Of these, 534 cases of preeclampsia and 847 normal healthy pregnant females investigated the significance of evaluation of NLR for identification of preeclampsia. The meta-analysis showed an overall significant effect in favor of the importance of NLR investigation in predicting preeclampsia (SMR = 1.04, 95% CI 0.91–1.16, p < 0.001). A significant Q statistic (p < 0.001) indicated the presence of heterogeneity (I2 = 96%). This systematic review and meta-analysis proved that NLR can be employed for detecting early preeclampsia. Further prospective studies are needed to validate the potential applicability of NLR as a diagnostic marker in clinical setup.
Keywords
Neutrophil-lymphocyte ratio
Preeclampsia
Pregnancy
Meta-analysis
Biomarker
INTRODUCTION
Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality among pregnant females. It is a pregnancy complication, occurring after 20 weeks of gestation, characterized by increased blood pressure and organ damage. Globally, it is the major cause of more than 70,000 maternal and 500,000 fetal deaths annually.[1,2] In India, the incidence of preeclampsia varies from 5% to 15%.[3]
The pathophysiology of preeclampsia is closely related to dysregulated immune response, with a characteristic increase in the pro-inflammatory immune cells and cytokines and vascular endothelial dysfunction.[4,5] Timely detection of pregnant females, who are at risk of developing preeclampsia becomes crucial and prudent to avoid adverse outcomes. Simple laboratory hematological parameters are worthy to be explored. Neutrophil-lymphocyte ratio (NLR) is a simple biomarker, evaluated using complete blood count. It reflects the status of the innate immune response, due to neutrophils and adaptive immunity, due to lymphocytes.[6] NLR has been widely explored in recent years as novel markers due to its prognostic value in diseases such as sepsis, atherosclerosis, pneumonia, COVID-19, and tumors.[7]
The literature review indicates the relationship between preeclampsia and NLR, but the results are contradictory and inconclusive.[8-10] Furthermore, no comprehensive review is available from Indian settings. Hence, the current meta-analysis was planned with the perspective to explore the NLR in preeclampsia and investigate its value for early diagnosis, assessment of severity, and prognosis.
MATERIAL AND METHODS
This study protocol was prospectively registered with PROSPERO and conducted with the requirements of the reporting rules in the “Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines”[11] and strictly complied with its specifications. Since this work is a systematic review, the heterogeneity was present within the acceptable range, meta-analysis was performed.
Eligibility criteria
Criteria for included studies were defined as adults aged ≥18 years and <40 years. The inclusion criteria based on the PICOS principle were as follows.
Population: Patients with preeclampsia of age ≥18 years <40 years diagnosed based on the standard criteria suggested by the American College of Obstetricians and Gynecologists as systolic blood pressure of 140 mmHg or more, or diastolic blood pressure of 90 mmHg or more on two occasions of at least 4 h apart along with proteinuria.[12]
Intervention (Exposure): High NLR
Control: Healthy pregnant females of age ≥18 years <40 years with no clinical symptoms or medications.
Outcomes: Diagnostic role of NLR
Studies: Case–control, cross-sectional, and longitudinal studies in Indian settings
Search strategy
Electronic retrieval methods were adopted for the literature retrieval. A comprehensive and systematic research review using a combination of Medical Subject Headings, controlled vocabulary, and keywords was conducted through various databases including PubMed, MEDLINE, and Google Scholar for studies till 2023. Furthermore, a manual search of a reference list of primary trials was conducted from the selected topics, and relevant articles were included in the review and analysis.
Study selection
The search results were uploaded into the online systematic review program Rayyan[13] to conduct the study selection. A two-stage screening process was conducted for study selection. Two independent authors (VD, KS) performed the literature search and screened the title, abstract, and keywords of all the studies. Screening of abstract and full text was done independently by three authors (VD, KS, and RM) to select the studies which satisfy the eligibility criteria of our review. Any disagreements or discordances present during the entire selection process were resolved either through consensus or consultation with the fourth author (JF). If conflicts arose between reviewers, the fifth reviewer (KG) moderated a discussion to come to a joint decision.
Data extraction and management
The relevant study characteristics for the review were extracted by the first and co-author independently related to outcome measures from the included studies. Data extraction was guided by a predetermined checklist with the first author last name, published year, total sample size, study design, study setting, study duration, study groups, age, blood pressure, body mass index (BMI), and NLR values [Table 1]. The obtained data is exported to the software Review Manager (RevMan_5.3, Copenhagen: The Nordic Cochrane Center, the Cochrane Collaboration, 2014).[14] Data entry was double-checked for correct entry by the second author (KS) through a comparison of data presented in the review and included in the reports.
| First Author | Year of publication | Study setting | Study design | Study period | Study population | PE Sample size | PE Age |
PE NLR |
NR Sample size | NR Age |
NR NLR |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Thombare et al. | 2023 | Hospital | Case–control | 24 months | 140 | 70 | 25.92±3.73 | 3.52±1.05 | 70 | 25.57±4.05 | 3.22±0.88 |
| Singhal et al. | 2019 | Hospital | Case–control | 10 months | 70 | 35 | >18 | 5.64±1.78 | 35 | >18 | 4.19±1.00 |
| Panwar et al. | 2019 | Hospital | Prospective nested case–control study | Not mentioned | 64 | 64 | Not mentioned | 5.55±0.81 | 376 | Not mentioned | 4.55±0.66 |
| Gogoi et al. | 2019 | Hospital | Cross-sectional study | 7 months | 134 | 67 | 28.5±5.6 | 6.8±7.6 | 67 | 27.8±5.5 | 3.0±0.98 |
| Gandham et al. | 2019 | Hospital | Prospective study | Not mentioned | 196 | 98 | 23.17±3.66 | 5.73±2.10 | 98 | 22.93±3.05 | 5.21±2.46 |
| Meena et al. | 2018 | Hospital | Comparative longitudinal study | 12 months | 100 | 50 | 27.60±6.47 | 7.39±3.51 | 50 | 26.98±6.33 | 3.20±1.08 |
| Sachan et al. | 2017 | Hospital | Prospective case–control | 12 months | 101 | 50 | 25.13±0.97 | 4.26±0.31 | 51 | 25.90±0.57 | 3.14±0.16 |
| Krishna and Manorama | 2018 | Hospital | Case–control study | 12 months | 200 | 100 | 27.60±6.47 | 7.39±3.51 | 100 | 26.98±6.33 | 3.20±1.08 |
PE: Preeclampsia, NR: Normal, NLR: Neutrophil-lymphocyte ratio
Outcome measure for the study
The outcome of the study is to explore the NLR in preeclampsia patients in Indian settings.
Quality assessment
The Joanna Briggs Institute approach was used to assess the risk of bias in the selected articles[15] and is shown in [Table 2].
| Case–control studies | Thombare et al. 2023 | Singhal et al. 2019 | Panwar et al. 2019 | Krishna and Manorama 2018 | Sachan et al. 2017 | Meena et al. 2018 | Gandham et al. 2019 | |
|---|---|---|---|---|---|---|---|---|
| Were the groups comparable other than the presence of disease in cases or the absence of disease in controls? | ||||||||
| Were cases and controls matched appropriately? | ||||||||
| Were the same criteria used for identification of cases and controls? |
||||||||
| Was exposure measured in a standard, valid, and reliable way? |
||||||||
| Was exposure measured in the same way for cases and controls? |
||||||||
| Were confounding factors identified? | ||||||||
| Were strategies to deal with confounding factors stated? | ||||||||
| Were outcomes assessed in a standard, valid and reliable way for cases and controls? | ||||||||
| Was the exposure period of interest long enough to be meaningful? |
||||||||
| Was appropriate statistical analysis used? | ||||||||
| Analytical Cross-sectional Studies (Gogoi P 2019) | ||||||||
| Were the criteria for inclusion in the sample clearly defined? | ||||||||
| Were the study subjects and the setting described in detail? | ||||||||
| Was the exposure measured in a valid and reliable way? | ||||||||
| Were objective, standard criteria used for measurement of the condition? | ||||||||
| Were confounding factors identified | ||||||||
| Were strategies to deal with confounding factors stated? | ||||||||
| Were the outcomes measured in a valid and reliable way? | ||||||||
| Was appropriate statistical analysis used? | ||||||||
JBI: Joanna Briggs Institute, Green Color-Yes, Red-No, Yellow-Unclear, Grey-Not applicable
Statistical analysis
A comprehensive qualitative analysis was made. For the quantitative meta-analysis, the binomial data were performed using RevMan_5.3.[14] Due to heterogeneity among studies, a logistic-normal random-effect model was conducted. The 95% confidence interval (CI) was performed for study-specific and overall pooled prevalence, respectively. To assess the heterogeny, I2 statistics were used. Significant heterogeny was considered if P < 0.05 or I2 >50% among the studies.
Subgroup analysis was performed to assess the heterogeneity and potential confounding for studies. Study-specific and pooled estimates were graphically represented through forest plots for both combined and subgroup analysis.
RESULTS
Study selection and characteristics
A total of 103 studies were initially retrieved from databases. After the removal of duplicates, a total of 54 studies were screened. Of those, eight studies met the inclusion criteria and were ultimately included in the qualitative and quantitative analysis.[16-23] The PRISMA flowchart for the study selection is shown in [Figure 1].
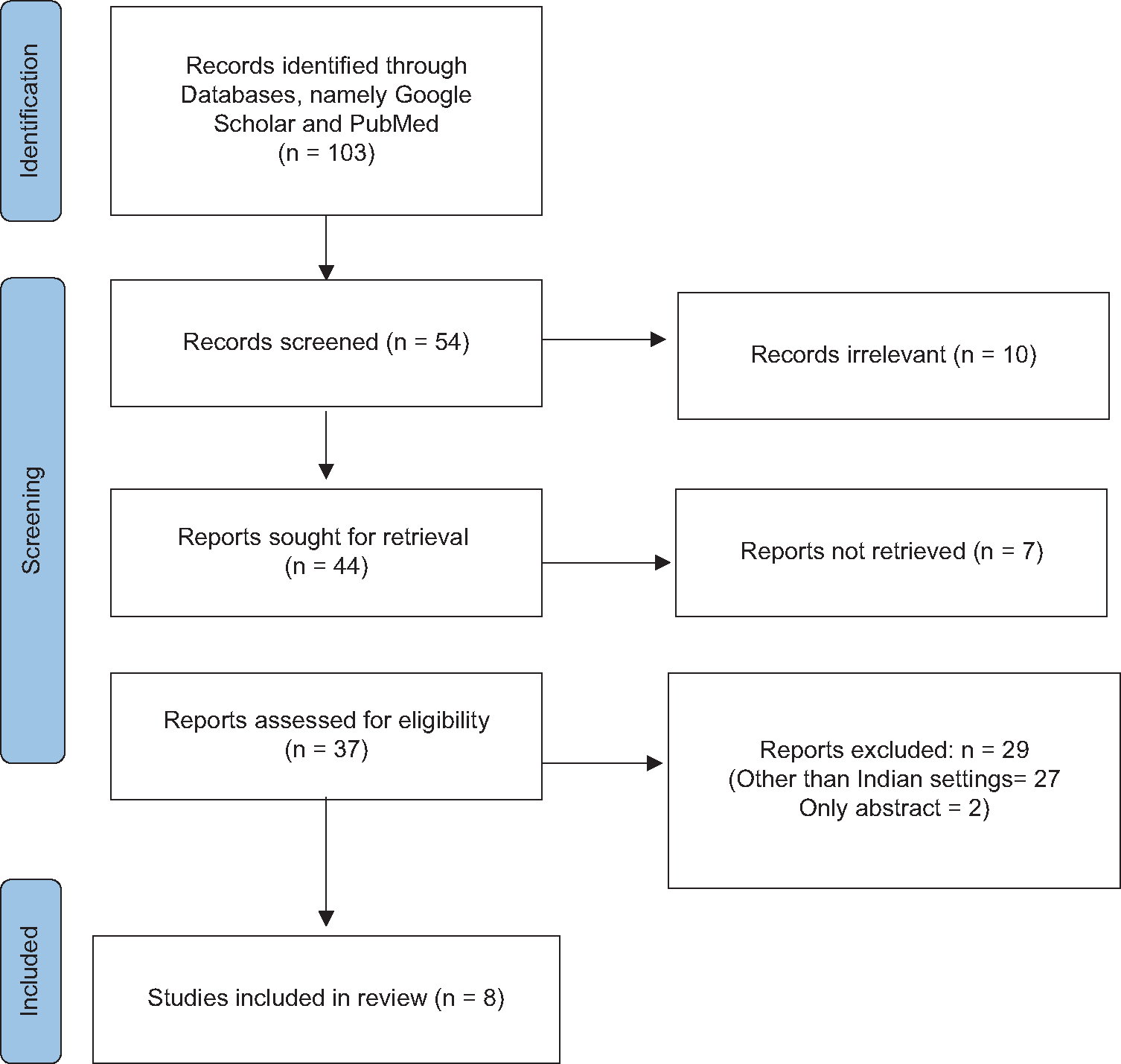
- PRISMA flow diagram of the study selection process.
Scope of reviewed studies
[Table 1] shows the details of the selected articles from Indian settings, from the year 2018 to 2023 in hospital settings. The study design belonged to three main categories, namely, case–control (five studies),[18,19,21-23] cross-sectional (one study),[17] and longitudinal study (two studies).[16,20]
Findings of the review
A meta-analysis of eight eligible comparing NLR in studies involving 534 subjects with preeclampsia and 847 normotensive pregnant mothers showed an overall significant effect in favor of the importance of NLR investigation in predicting preeclampsia (SMR = 1.04, 95% CI 0.91–1.16, P < 0.001), as shown in [Table 1]. A significant Q statistic (P < 0.001) but the presence of heterogeneity (I2 = 96%) was found, as shown in [Figure 2].

- The size of the square box is proportional to the weight that each study contributes in the meta-analysis. The overall estimate and confidence interval are marked by a diamond.
DISCUSSION
The current systematic review and meta-analysis involving 8 studies including 1381 study population, with 534 cases of preeclampsia and 847 normal healthy pregnant females investigated the significance of evaluation of NLR for identification of preeclampsia. In recent years, NLR has gained attention reflecting the systemic inflammatory response. A review represents that evaluating the angiogenic factors with or without clinical features can help in predicting early- and late-onset preeclampsia.[24] Similarly, another study suggests a new model for screening early-onset preeclampsia based on the maternal characteristics, serum pregnancy-associated plasma protein-A and placental growth factor, mean arterial pressure, and uterine artery pulsatility index.[25] NLR is a simple hematological routine biomarker that is cost-effective and is used for early detection of preeclampsia.[26]
The diagnostic accuracy and prediction of preeclampsia using NLR in the selected Indian settings using sensitivity, specificity, and area under curve (AUC) were analyzed in three studies.[19,21,23] A meta-analysis evaluating the diagnostic accuracy of NLR in 1298 preeclampsia patients reported the diagnostic odds ratio as 8.44 (95% CI 4–17.78) and AUC as 0.82.[27]
In the present meta-analysis, it is reported that NLR has significant value in predicting preeclampsia. Similar results are also reported in other studies.[28-30] In normal pregnancy, neutrophils increase 2.5 folds by 30 weeks of gestation and the increase is more pronounced in preeclampsia, which is supposed to be due to increased levels of colony-stimulating factors.[31,32] A study conducted by Serin et al., in 2016, reported that NLR was significantly higher in severe preeclampsia compared to mild preeclampsia which suggests that NLR could be employed to predict the severity of preeclampsia. Activation of immune cells and inflammation releases reactive oxygen species and cytokines leading to endothelial dysfunction.[33]
To the best of our knowledge, the current systematic review and meta-analysis is the first of its kind done in Indian settings. It is evident that NLR can be considered as a useful, inexpensive, and fast biomarker for preeclampsia. There were some limitations in the study like, the number of studies included was limited, lack of randomized trials, information like gestational age, AUC, BMI, and blood pressure were not reported in all studies, which in case if provided would have added value to data analysis.
CONCLUSION
The meta-analysis suggests that NLR can be employed as a useful hematological marker for the prediction and evaluation of preeclampsia. However, other crucial factors should also be taken into consideration that can alter NLR in preeclampsia. Further larger multi-centered longitudinal studies can help us in predicting the timings and cutoff values for preeclampsia in clinical setup.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24-43.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertensive disorders in pregnancy. Indian J Anaesth. 2018;62:675-81.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokine imprint in preeclampsia. Front Immunol. 2021;12:667841.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil to lymphocyte ratio: An emerging marker of the relationships between the immune system and diseases. Int J Mol Sci. 2022;23:3636.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil-to-lymphocyte ratio as a predictor of disease severity and mortality in coronavirus disease 2019: Prospective study from central India. Cureus. 2022;14:e23696.
- [CrossRef] [Google Scholar]
- Prediction of preeclampsia by first trimester combined test and simple complete blood count parameters. J Clin Diagn Res. 2015;9:C20-3.
- [CrossRef] [PubMed] [Google Scholar]
- Are neutrophil/lymphocyte ratio (NLR), platelet/ lymphocyte ratio (PLR), and/or mean platelet volume (MPV) clinically useful as predictive parameters for preeclampsia? J Matern Fetal Neonatal Med. 2019;32:1412-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, mean platelet volume, red cell distribution width and plateletcrit in preeclampsia. Pregnancy Hypertens. 2017;7:29-32.
- [CrossRef] [PubMed] [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- [CrossRef] [PubMed] [Google Scholar]
- ACOG Practice Bulletin No. 222 Obstet Gynecol. . 2020;135:e237-60.
- [CrossRef] [PubMed] [Google Scholar]
- Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
- [CrossRef] [PubMed] [Google Scholar]
- RevMan 5. Available from: https://training.cochrane.org/online-learning/core-software/revman/revman-5-download [Last accessed on 2022 Jul 07]
- [Google Scholar]
- The Joanna Briggs Institute approach for systematic reviews. Rev Lat Am Enfermagem. 2018;26:e3074.
- [CrossRef] [Google Scholar]
- A comparative study to assess relation of platelet count, neutrophil and lymphocyte ration as predictor of pre-eclampsia in normotensive and pre-eclamptic women. Int J Clin Obstet Gynaecol. 2018;2:86-8.
- [CrossRef] [Google Scholar]
- Neutrophilto-lymphocyte ratio and platelet indices in pre-eclampsia. Int J Gynaecol Obstet. 2019;144:16-20.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in antenatal women with pre-eclampsia: A case-control study. Cureus. 2023;15:e40338.
- [CrossRef] [Google Scholar]
- Neutrophil lymphocyte ratio (NLR) as a bio inflammatory marker in preeclampsia. Int J Contemp Med Res. 2019;6:4-6.
- [CrossRef] [Google Scholar]
- Neutrophil and platelet to lymphocyte ratio in prevailing the oxidative stress and its relation with the endothelial dysfunction in preeclampsia. J Krishna Inst Med Sci Univ. 2019;8:89-97.
- [Google Scholar]
- Diagnostic accuracy of neutrophil to lymphocyte ratio in prediction of nonsevere preeclampsia and severe preeclampsia. J Curr Res Sci Med. 2017;3:79.
- [CrossRef] [Google Scholar]
- A study on role of neutrophil to lymphocyte ratio as predictor of pre eclampsia. IOSR J Dent Med Sci. 2018;17:1-4.
- [Google Scholar]
- Raised neutrophil lymphocyte ratio and serum beta hCG level in early second trimester of pregnancy as predictors for development and severity of preeclampsia. Drug Discov Ther. 2019;13:34-7.
- [CrossRef] [PubMed] [Google Scholar]
- Combining biomarkers to predict pregnancy complications and redefine preeclampsia: The angiogenic-placental syndrome. Hypertension. 2020;75:918-26.
- [CrossRef] [PubMed] [Google Scholar]
- A new model for screening for early-onset preeclampsia. Am J Obstet Gynecol. 2020;222:608.e1-18.
- [CrossRef] [PubMed] [Google Scholar]
- Role of derived neutrophil-to-lymphocyte ratio, uric acid-to-creatinine ratio and Delta neutrophil index for predicting neonatal outcomes in pregnancies with preeclampsia. J Obstet Gynaecol. 2022;42:1835-40.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic value of neutrophil-lymphocyte ratio in preeclampsia: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e18496.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil lymphocyte ratio and red cell distribution width as a marker of preeclampsia: A retrospective study. J Preg Child Health. 2017;4:307.
- [CrossRef] [Google Scholar]
- High first-trimester neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios are indicators for early diagnosis of preeclampsia. Ginekol Pol. 2016;87:431-5.
- [CrossRef] [PubMed] [Google Scholar]
- Is neutrophil/lymphocyte ratio a useful marker to predict the severity of pre-eclampsia? Pregnancy Hypertens. 2016;6:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the differential distribution of leukocytes in preeclampsia versus uncomplicated pregnancy. Gynecol Obstet Invest. 1998;45:229-31.
- [CrossRef] [PubMed] [Google Scholar]
- Elevation of serum macrophage colony-stimulating factor before the clinical manifestations of preeclampsia. Am J Obstet Gynecol. 2003;189:1356-60.
- [CrossRef] [PubMed] [Google Scholar]
- ICSH Guideline for worldwide point-of-care testing in haematology with special reference to the complete blood count. Int J Lab Hematol. 2008;30:105-16.
- [CrossRef] [PubMed] [Google Scholar]








