Translate this page into:
Normal variations in MR venography that may cause pitfalls in the diagnosis of cerebral venous sinus thrombosis

*Corresponding author: Elamparidhi Padmanaban, Department of Radiology, Sri Manakula Vinayagar Medical College, Puducherry, India. pepsantosh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thomas RK, Padmanaban E, Raj JV, Varadane A, Sambath P. Normal variations in MR venography that may cause pitfalls in the diagnosis of cerebral venous sinus thrombosis. Glob J Health Sci Res 2023;1:22-6.
Abstract
Objectives:
Magnetic resonance venography (MRV) is a widely used non-invasive imaging technique to diagnose cerebral dural venous sinus thrombosis (CVST) and intracranial venous abnormalities. Non-visualization of a dural venous sinus is diagnostic of CVST on MRV. However, there are numerous common variances and technical aberrations on MRV that mimic filling defects and might be confused with CVST, making diagnosis difficult. These include aberrant veins and missing, hypoplastic or asymmetric venous sinuses. In addition, reconstruction artifacts might take the form of flow gaps with various lengths. The purpose of this study is to examine the occurrences, geographic distribution, and imaging properties of these variations and artifacts on MRV.
Materials and Methods:
After obtaining clearance from the Institution’s Ethics Committee, magnetic resonance imaging (MRI) brain of 60 patients were taken for the study. MRI was performed using 1.5 Tesla Intera PHILIPS. A cross-sectional study was conducted to study the normal anatomy of the intracranial venous system and its normal variations.
Results:
This study showed that hypoplasia of the left transverse sinus was found to be more predominant (60%) among other sinuses of the brain followed by right transverse sinuses (31%); the left sigmoid sinus was hypoplastic in 35%, the right sigmoid sinus hypoplastic in 18% and superior sagittal sinuses in 5%.
Conclusion:
It is essential to know the anatomical variations of the dural venous system for the discrimination between pathological processes such as thrombosis and physiologic conditions. Furthermore, the association of these variations with each other must be kept in mind for explanation of the presence of multiple variations in the same individuals.
Keywords
Cerebral dural venous sinus thrombosis
Magnetic resonance imaging
Superior sigmoid sinus
Transverse sinus
INTRODUCTION
Magnetic resonance venography (MRV) is a widely used noninvasive imaging technique to diagnose cerebral dural venous sinus thrombosis (CVST) and intracranial venous abnormalities. The diagnosis of cerebral venous sinus thrombosis on MRV primarily depends on nonvisualization of a venous sinus or a segment appearing like a filling defect. However, there are many normal variations and technical artifacts occurring on MRV simulating filling defects which can mimic cerebral venous sinus thrombosis causing diagnostic pitfalls. These include absent, hypoplastic or asymmetric venosus sinuses and anomalous veins. Furthermore, reconstruction artifacts can appear as flow gaps of different lengths. This study aims to study the frequencies, location and imaging characteristics of these variations and artifacts on MRV.
Blood clot within the brain’s venous sinuses results in cerebral venous sinus thrombosis. This results in stasis of blood within the venous sinus later leading to brain parenchymal hemorrhage. Due to pregnancy, puerperium and use of oral contraceptive pills, it frequently affects patients who are young to middle aged, notably women in the age range of 20–35.
There are numerous causes that can lead to cerebral venous sinus thrombosis, and a patient will frequently have more than one of these conditions. The most common causes include genetic conditions such as antithrombin deficiency, protein C and protein S deficiency, Factor V Leiden, antiphospholipid antibody, acquired conditions such as nephritic syndrome, pregnancy and puerperium, infective causes such as otitis, mastoiditis, sinusitis, and meningitis, systemic lupus erythematosus, sarcoidosis, drugs such as oral contraceptives and tamoxifen, and systemic causes such as septicemia, endocarditis, typhoid and tuberculosis.
MATERIAL AND METHODS
This study was carried out in the Department of Radiodiagnosis, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India. It is a hospital-based prospective study. After obtaining clearance from the Institute’s Ethics Committee, 60 cases who were referred to the department of radiodiagnosis for magnetic resonance imaging (MRI) brain during the period of July 2021–2022 were analyzed.
An MRI study was performed on 1.5 Tesla Intera PHILIPS whole body magnetic resonance (MR) systems using standard imaging head coil.
Inclusion criteria
The following criteria were included in the study:
Clinically suspected cases of intra-cranial vascular lesions who were referred to radiology department for MRI brain with venography
Known cases of CVST.
Exclusion criteria
The following patients were excluded from the study:
Patients with contrast allergy
Patients with metallic prosthesis, cochlear implants
Patients with claustrophobia
Patients with pacemakers
Patient with MR-incompatible prosthetic heart valves.
RESULTS
Patients with a range of symptoms were included in the study. The total number of patients included in the study was 60, which included 22 males and 38 females [Chart 1]. The median age of participants is 50 years, with age ranging from 20 to 70 years. Moreover, the same pattern continues to follow among both the sexes. [Table 1] clearly shows that 28.1% among females and 27.8% among males were falling in the age group of 21–30 years with CVST. Whereas, only 3% were in the age group of 61–70 in both cases.
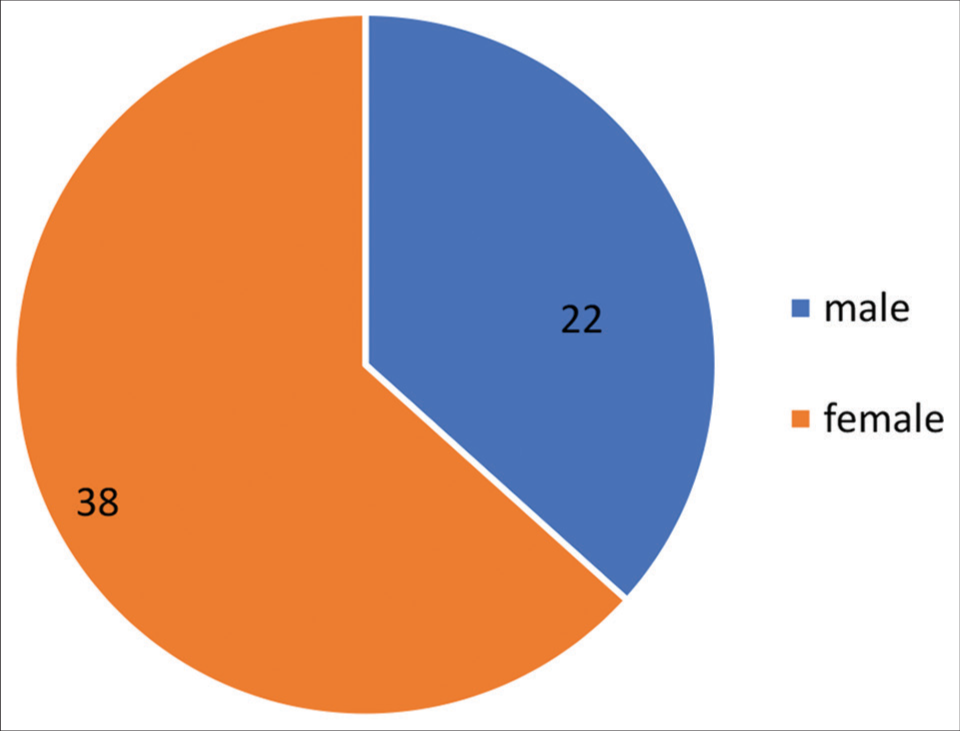
- A pie chart representing gender distribution of cerebral dural venous sinus thrombosis.
| Age years | Number of subjects | Relative frequency |
|---|---|---|
| 11–20 years | 9 | 0.15 |
| 21–30 years | 18 | 0.30 |
| 31–40 years | 11 | 0.18 |
| 41–50 years | 9 | 0.15 |
| 51–60 years | 10 | 0.16 |
| 61–70 years | 3 | 0.05 |
The superior sagittal sinus (SSS), the vein of Galen, the internal cerebral vein and the straight sinus were observed constantly in almost all patients. In the transverse sinus, the right dominance, left dominance, and codominance were noted in 31%, 65%, and 4%, respectively. The left transverse sinus (LTS) was hypoplastic in 49% and aplastic in 11%. The right transverse sinus (RTS) was hypoplastic in 31% [Chart 2]. The occipital sinus was present in 5% and was associated with a hypoplastic or aplastic transverse sinus providing alternative drainage pathways from the straight sinus to the internal jugular vein.

- Bar diagram showing distribution of patients with normal cerebral venous sinus variants.
Hypoplastic LTS was found to be more predominant in 60% among other sinuses of the brain followed by RTSs in 31%, left sigmoid sinus hypoplastic in 35% and right sigmoid sinus hypoplastic in 18% and SSSs in 5%.
DISCUSSION
On MRV, common variations in venous anatomy can be seen. Most common indication to get MRV of brain was headache in this study. To assess the presence and relative size of the transverse dural sinus in contrast to the SSS, MRV was performed. Normally, the RTS receives drainage from the SSS. Dominant transverse sinuses are those that receive the SSS. Compared to other brain sinuses, the LTS [Figure 2] was shown to be more prevalent (60%) [Table 2]. Next was RTSs with 31%, and SSSs with 5% [Figure 4]. Transverse sinus atresia and hypoplasia are prevalent. These results agree with Goyal et al.[1] who described the transverse sinus anatomical variations as follows; 66.9% bilateral symmetrical transverse sinus, 21.3% LTS hypoplasia, 4.1% aplastic left sinus [Figure 3], 5.5% hypoplastic RTS, and 0.7% aplastic RTS [Table 2]. Technical artifacts in MRV happen during reconstruction and as a result of incorrect data registration. These are additionally typically observed in clinical MR imaging. Transverse sinus flow gaps can be mistaken as flow gaps is cerebral venous thrombosis.

- Normal anatomy of the cerebral venous system.

- Phase-contrast magnetic resonance venography in a 45-year-old female patient with idiopathic intracranial hypertension. Maximum intensity projection demonstrates left transverse sinus hypoplasia.

- Magnetic resonance venography in a 62-year-old female patient with transverse myelitis. Maximum intensity projection demonstrates left transverse sinus aplasia.

- Magnetic resonance venography in a 38-year-old male patient with multiple tuberculomas. Maximum intensity projection demonstrates right transverse sinus aplasia.
| Sinuses involved | No. of cases with hypoplastic sinus | Percentage |
|---|---|---|
| Superior sagittal sinus | 3 | 5 |
| Left transverse sinus | 36 | 60 |
| Right transverse sinus | 19 | 31 |
| Left sigmoid sinus | 21 | 35 |
| Right sigmoid sinus | 11 | 18 |
The occipital sinus, the smallest of the dural venous sinuses, connects the torcula with the internal jugular vein and can be single, duplicated, or made up of a network of venous collaterals. In a study conducted by Ayanzen et al.[2-4] of 100 children, persistent occipital sinuses were seen in 13% of patients <25 months of age but in only 2% of children older than 5 years. This study lends credence to the idea that the occipital sinus will involute once the infant is standing upright and the majority of the venous flow has passed through the big dural sinuses. In our study, 4% of the patients had an occipital sinus found. The overreporting of occipital sinus incidence in the literature may be due to misclassification of other venous structures as the occipital sinus or racial variances in the populations under study.[5]
Alper et al. conducted a different study that listed the anatomical variations of the transverse sinuses as follows: 39% LTS, 31% bilateral symmetrical transverse sinus, 20% aplastic LTS, 6% hypoplastic RTS and 4% aplastic RTSs.[3]
Surendrababu et al. conducted a second study in which they described the anatomical differences of the transverse sinus as follows: 1% of patients had aplastic LTS, 35% had LTS, 13% had hypoplastic RTS, and 10% had bilaterally symmetrical transverse sinuses.[4]
CONCLUSION
Cerebral venous thrombosis is a relatively uncommon but serious neurologic disorder. The diagnosis method is primarily based on imaging. Because venous thrombus formation and brain parenchymal changes may be reversible, prompt and proper medical therapy is crucial. Combination of a small sinus size, a slow or complex flow pattern, an image acquisition plane not parallel to the sinus could be the likely causes for misdiagnosis of CVST.[6] Therefore, these variants and artifacts can be potential pitfalls in the MRV diagnosis of CVST specially where there are no supportive imaging features such as brain infarcts.[6,7] To prevent making an incorrect diagnosis of sinus thrombosis, it is crucial to understand the anatomical variations of the cerebral dural venous sinuses. In our present study, LTS is by far the most frequent anatomical variant found.
Acknowledgment
I acknowledge with a deep sense of gratitude my guide Dr. Elamparidhi, Associate Professor, for his constant guidance and encouragement. His dedication towards work will always be a constant source of inspiration.
I am indebted to my Associate and Assistant Professors and my fellow postgraduate residents for all the help and assistance that I received while doing this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Anatomical variations of cerebral MR venography: Is gender matter. Neurointervention. 2016;11:92-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral venography: Normal anatomy and potential diagnostic pitfalls. AJNR Am J Neuroradiol. 2000;21:74-8.
- [Google Scholar]
- Importance of anatomical asymmetries of transverse sinuses: An MR venographic study. Cerebrovasc Dis. 2004;18:236-9.
- [CrossRef] [PubMed] [Google Scholar]
- Variations in the cerebral venous anatomy and pitfalls in the diagnosis of cerebral venous sinus thrombosis: Low field MR experience. Indian J Med Sci. 2006;60:135-42.
- [CrossRef] [PubMed] [Google Scholar]
- High-resolution MR venography of cerebral arteriovenous malformations. Magn Reson Imaging. 1999;17:1417-25.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral transverse sinus morphology as detected by MR venography in patients with chronic migraine. Headache. 2012;52:1254-61.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative evaluation of 2D time-of-flight and 3D elliptic centric contrast-enhanced MR MR venography in patients with presumptive cerebral venous and sinus thrombosis. Eur J Neurol. 2007;14:139-43.
- [CrossRef] [PubMed] [Google Scholar]







