Translate this page into:
The mechanical cause of loculated pleural effusion

*Corresponding author: Nikhil Mishra, Department of General Medicine, Kyrgyz State Medical Academy Kyrgyzstan, Bishkek, Kyrgyzstan. nikhilishere843@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mishra N. The mechanical cause of loculated pleural effusion. Glob J Health Sci Res 2023;1:38-40.
Abstract
In this research, we are going to deal with the probable mechanism behind the loculated pleural effusions using the Law of Viscous fluids against rough surfaces/walls. The idea of the research is to form a firm ground regarding the mechanism of pleural effusion.
Keywords
Loculated pleural effusion
Pleural effusion mechanism
Pleural effusion classification
INTRODUCTION
As we know by now pleural effusions are caused due to a particularly large number of underlying pathologies such as pneumonia which accounts to almost 53% of cases, tuberculosis, congestive heart failures, cirrhosis, and a lot more. The point of discussion of this research is particularly loculated pleural effusion which can either be transformed into malignancy and have a poorer prognosis or empyema which if may left behind after the chest tube drainage can sure shot lead to malignancy or further reoccurrence of disease or some other fatal infections.
Regarding locular effusion, the most uncommon or unorthodox behavior of the fluid is what that draws the major attention by forming atypical shapes that are observable on CT’s, radiographs, and USG which is still needed to be understood.
CLASSIFICATION OF EFFUSION
For this, we have classified effusion on the basis of pleural fluid positivity and gram stain positivity and also pH [Chart 1].
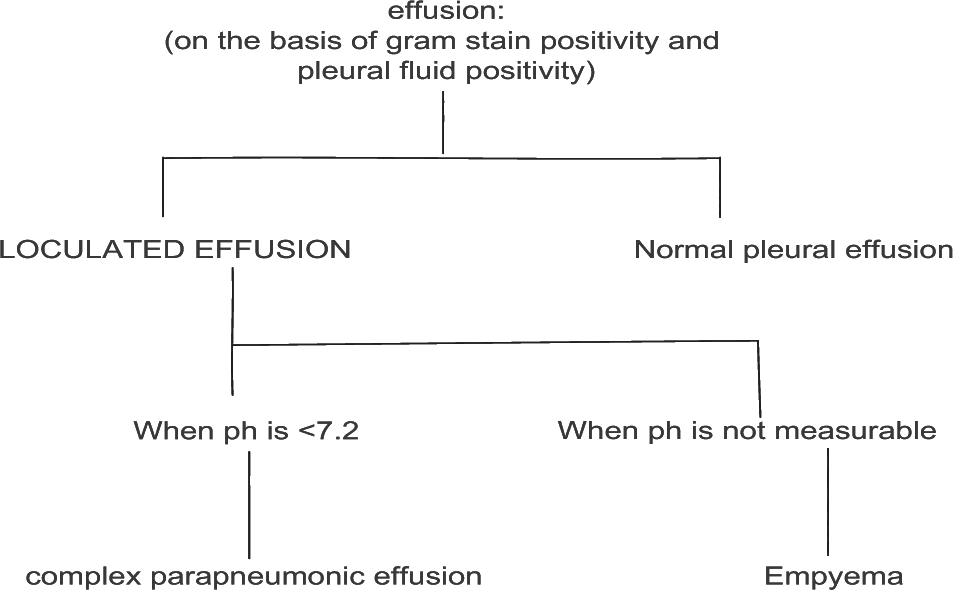
- Classification of effusion on basis of pleural fluid and gram stain positivity and also pH.
Complex parapneumonic effusion and empyema both are the fluids/liquids that contains a good amount of (more than usual) of leukocytes. Hence, it makes the fluid grainy or to be said viscous/ turbid which is also verified when drained out through chest tubes as they are straw colored may be hemorrhagic but surely turbid.
In the pleural cavity, as suggested, there are mesothelium cells which are responsible for surfactant secretion and certain lymphatics which help in generating a negative pressure during rest.
Presence of certain cells on the parenchyma of the lungs or the chest walls, it is really hard to consider the walls of these surfaces (constituting to the pleural cavity) as “ideally smooth surfaces.”
According to the wall laws for viscous fluid near rough wall surfaces, we should consider the wall law of first order which is the Dirichlet law that states, a fluid satisfies a “no slip” boundary conditions under the homogenized surface. Furthermore, we should take in the consideration of the type of the fluid associated with law or experiment.
CASE SERIES
CASE 1
Presence of any non-viscous liquid/fluid like water (may or may not be macroscopically clear) or transudates.
As these are non-viscous liquids/fluids and are less denser, these do not correspond to the law and hence will now follow “no slip” boundaries or rather will follow “slip” boundaries.
Hence are least likely to develop into loculated pleural effusion [Figure 1].

- (a) This is the CXR of pleural effusion caused by transudate showing no special pattern of fluid. Hence, a normal pattern is obtained. (b) This is the USG of pleural effusion caused by transudates.
CASE 2A
Presence of parapneumonic fluid or empyema (viscous liquids) or exudates in normal healthy pleural cavity [Figure 2].
As these fluids clearly follow the wall law of first order and are coherent to all the conditions of rough surfaced walls are likely to have a loculated approach.
According to the law when the edges of the fluid comes into the contact of the parenchyma of the lung surface and the chest wall they tend to have a “no slip” movement.

- (a) CXR of loculated pleural effusion showing the unique pattern. (b) USG of loculated pleural effusion showing the unique pattern.
During inspiration and expiration, due to the compensatory movement of the chest wall in response to the lungs, the surface area between them tend to change frequently, these fluids when present inside the cavity have a pulsating affect due to frequent change in the surface area caused by inspiration and expiration and hence splash/rise to a certain height on either side of the wall. As these fluids show no slip movement they tend to “adhere” to the surface they reached by pulsation and hence carry on their journey from there for the next pulsation.
As these pulsation that are generated as a change in surface area is not that determining macroscopically, small gradual movements are made by these fluids over the time.
When a typical amount of fluid (say 40–60 mL) is accumulated, pleural effusion starts showing its classical symptom of dyspnea. As the pulsation continues, the shortness of breath here is the positive feedback for the localization to happen as the shortness of breath increases the repetition of pulsation and demise the time interval between two consecutive pulsation, the frequency of pulsation increases hence giving the fluid to localize in much better conditions than before but using the same principle as before.
CASE 2B
Presence of parapneumonic fluid or empyema (viscous fluids) in a non-healthy pleural cavity.
Let’s consider two cases under this case.
Case 2B (i)
Lung/chest wall parenchymal damage due to certain pathology resulting in the depletion/irregularity of the surfaces.
Due to the unevenness/irregularities which is incremental in this condition, the localization is most likely to happen. For the viscous fluids to adhere to the wall, one of the most primary cause is the type of surface and the level of roughness it offers. Here, as the roughness is increased quite significantly and also as the symptom dyspnea is followed, it provides the most premium condition for the fluids to localize and hence the rise of the fluid in the definite shape is more significantly observed macroscopically.
Case 2B (ii)
Lack of mesothelium cells/improper functioning of the cells.
As these cells are responsible for the secretion of the surfactant which actually provides cushioning to the lungs, have some immediate effect on making the surfaces relatively smoother.
Due to improper functioning of cells/lack of these cells, relatively much lesser surfactant is present leading to the further roughness of the surfaces and hence leading to the condition that is same followed as CASE 2B (i).
CASE 3
Presence of fluids in the fibrotic pouches created in the parenchyma due to the tear of lesions [Figure 3].
Sometimes due to the tear of fibrotic lesions in the parenchyma, some slits and pouches are created. Deposition of these fluids in the pouches processes a loculated pleural effusion. Although presence of parapneumonic fluid increases the morbidity ratio as it is quite infectious by nature and degrades the prognosis quite a few times.

- CXR of loculated pleural effusion (trapped) in pouch created.
NOTE
The laws of viscous fluid near rough wall are technically applicable to the parts of flow that are close to the walls that is <20% of the height of flow. During the course of research, this consideration was taken into account.
Patients on diuretics can be misjudged as exudates instead for transudates. Hence, proper history taking is advisory.
INVESTIGATION
Investigation should be carried out according to the recent guidelines.
CONCLUSION
The loculated pleural effusion can lead to various dreadful sequalea, the pathogenesis of which has to be explored further through the research.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.







