Translate this page into:
Effect of the lunar cycle on mental illness – A single-center retrospective observational study

-
Received: ,
Accepted: ,
How to cite this article: Radhakrishnan S, Selvaraj A, Sivakumar P, Kulothungan V, Sathiyamoorthy P. Effect of the lunar cycle on mental illness – A single-center retrospective observational study. Glob J Health Sci Res 2023;1:161-7.
Abstract
Objectives:
In Shakespeare’s play “Othello,” the maid Emilia tells Othello that the moon has drawn too close to the Earth — and driven men insane. The notion that a full moon can elicit strong emotions, strange behavior, and even physical disease is not merely literary. Even now, it is a deeply held notion. The goal of this study was to determine the effect of the lunar cycle on the psychiatric presentation of individuals with schizophrenia, BPAD mania, and ATPD.
Material and Methods:
Case files of Schizophrenia, bipolar affective disorder (BPAD) mania and psychosis patients admitted in our hospital during full moon and new moon ± 3 days for the past 5 years will be included in the study. Name, age, sex, duration of admission, worsening of symptoms during full moon day and new moon day, any injectable given or not will be noted. These data will be collected from medical records. Telephonic verification of symptom worseness during full moon and new moon will be done.
Results:
Among 207 participants 74 patients had Schizophrenia, 91 patients had BPAD mania, 25 patients had ATPD and 17 patients had acute psychosis. The exacerbation of psychiatric symptoms, chemical restraints, and admission during phases of moon was statistically associated with lunar patterns in the study population. The rest of the socio-demographic factors, duration of admission, caregiver belief, and symptom worsening noted by caregiver were all not associated with mental illness during lunar phases which is in line with most reported literature in this area.
Conclusion:
There was an association between symptom exacerbations, chemical restraints, admission with different lunar phase. There was no association for sociodemographic details, duration of admission, caregiver belief on symptom worsening, symptom worsening noted by caregiver with different lunar phases.
Keywords
Full moon
New moon
Lunar phase
INTRODUCTION
The association of lunar phases with altered mental state of humans and animals is a historic topic. There exist many beliefs, even today that the moon has an effect on the behavior of people and more so on mental health. There is an ongoing debate concerning the connection between the lunar cycle and psychiatric illness. In fact, one study says that nearly 81% of mental health professionals believe the full moon can make people ill.[1] There is a popular belief that lunar periodicity influences animal physiology and behavior such as foraging, fecundity, melatonin secretion, thermoregulation patterns, and attacks on humans. Previous studies on the relationship between the moon phase and disease occurrence and aggravation, sleep quality, and incidence of accidental injuries indicate that human physical and mental states are also affected by the lunar cycle.[2] Suicidal behavior and suicidal risk which are important determinants of mental health are linked to and seasonal change.[3] There exists evidence from research that had overestimated the effect of the full moon phase on psychiatric presentations, which has limited the amount of information on all four lunar phases.[1]
The relationship between the association of lunar phases and mental illness is complex and ambiguous. A secondary research stated that on filtering based on the effect-size estimates, the phases of the moon accounted for no more than 1% of the variance in activities usually termed lunacy.[4] This is further endorsed by other studies that proved no significant relationship existed in this aspect.[5,6] However there is documented evidence for a defined relationship, between suicide rates and admission during lunar phases as well.[7,8] A hospital-based study identified records of sentinel events, like the requirement of a physical restraint and chemical restraint, occurring on full moon days, new moon days, and control days. They have recorded that sentinel events, such as the use of restraints, especially chemical ones, in psychiatrist in-patients are significantly more common during the full moon and new moon phases.[9] Adding to the controversy is a Finnish study that showed that no correlation between suicides and moon phase in any season was apparent for male victims, but a significant factor considering in winter for women underscoring seasonal and sex variations to be contributing factors in this subject.[10]
There are minimal studies that probed all possible socioeconomic factors along with disease which primarily reflect psychosis (rather than symptoms such as depression and anxiety) being studied for associations with lunar phases. We attempted to analyze this relationship in Indian participants for schizophrenia, bipolar affective disorder (BPAD) mania, and acute and transient psychotic disorder (ATPD) with all the phases of moon tracking on links from both sociodemographic and clinical patterns.
MATERIAL AND METHODS
Study settings and sample
A single-center retrospective study was conducted from March 2022 to September 2022 at the Department of Psychiatry, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry. The ethical clearance was obtained (Ref no: EC/35/2022) before the commencing of the study.
The study included medical records of patients with Schizophrenia, BPAD mania, and ATPD patients admitted to our hospital during the full moon and new moon ± 3 days over the past 5 years. The sample size was calculated using the software Open-Epi (version 3.01) to be 207. The sample technique adopted was convenient sampling.
Those patient medical records with diagnosed mental illness as “Schizophrenia” OR “BPAD mania” OR “ATPD,” those admitted in stated hospital during the full moon and new moon ± 3 days over a stated time frame (5 years from point of data collection) were included in the study. Schizophrenia, BPAD mania, and ATPD patient records with incomplete data or missed data during the full moon and new moon ± 3 days were excluded from the study.
Data collection
Schizophrenia, BPAD mania, and ATPD patients admitted during the full moon and new moon ± 3 days over the past 5 years were taken for the study. The demographic variables such as name, age, sex, duration of illness, address, date of admission, duration of admission, date of discharge, and symptom worsening during full moon day and new moon day. During worsening of symptoms during full moon day and new moon day, any injectable given were noted. Symptom worsening during full moon/new moon taken into account medical record if the patient had symptom exacerbation ± 3 days from admission. These data collected pertaining to the dates of admission were verified by telephonic interviews for confirmation as needed. The data collected from standard pro forma were entered in Excel sheets and subjected to statistical analysis.
Statistical analyses
The data were analyzed using the software Epi-Info, version 7.2.1.0, SPSS version 24. Microsoft Excel will be used to generate graphs, charts, and tables. Variables were compared using Independent t-test for discrete data and Chi-square test for continuous data.
RESULTS
A total of 207 medical records were retrospectively analyzed for understating the association of all lunar phases with stated sociodemographic and clinical patterns of Schizophrenia, BPAD mania, ATPD. Associations were tested using a Chi-square and P < 0.05 was considered significant.
Characteristics of the study population
The age distribution of the participants showed that a higher proportion of the participants were in 20–29 years (38.6%) followed by 30–39 years (23.7%), 40–49 years (16.4%), 50 years and above(12.6%) and below teenage was 8.7%. The study population consisted of 58% of males and 42% of females. Among the participants, 107 (51.7%) were unmarried, 96 (46.4%) were married and 4 (1.9%) were widows/widower. A majority of the participants were graduates (35.7%) and almost one-fourth were secondary and higher secondary each. Among the participants, 40.1% were unemployed and most belonged to the middle class. Considering the disease status, 74 (35.7%) had schizophrenia, 91 (44%) had BPAD mania and 42 (20.3%) had psychosis. The association of these variables with different types of mental illness under the four lunar phases is shown in [Table 1].
Associations of lunar phase with sociodemographic details
The proportion of mental illness at the new moon around 3 days was high in both males (52.5%) and females (48.3%), respectively. However, there was no association between sex and different lunar phases (χ2 = 3.029, df = 3, P = 0.387). Likewise, marital status. (χ2 = 4.64, df = 6, P = 0.510), educational status (P = 0.675), employment status of the patients (P = 0.094), and socioeconomic status (P = 0.507) were not significantly associated with schizophrenia, BPAD mania and ATPD. The above table shows there was a significant association was present between psychiatric admission and lunar phases (P < 0.001) [Table 1].
| Variables | Full moon n (%) |
Full moon±3 days n (%) |
New moon n (%) |
New moon±3 days n (%) |
Total n (%) |
χ2 | df | P-value |
|---|---|---|---|---|---|---|---|---|
| Admission | 15 (7.2) | 74 (35.7) | 13 (6.3) | 105 (50.7) | 207 (100.0) | 119.47 | 3 | 0.001 |
| Gender | ||||||||
| Male | 11 (9.2) | 38 (31.7) | 8 (6.7) | 63 (52.5) | 120 (100.0) | 3.029 | 3 | 0.387 |
| Female | 4 (4.6) | 36 (41.4) | 5 (5.7) | 42 (48.3) | 87 (100.0) | |||
| Marital status | ||||||||
| Married | 7 (7.3) | 37 (38.5) | 3 (3.1) | 49 (51.0) | 96 (100.0) | 4.64 | 6 | 0.510 |
| Unmarried | 8 (7.5) | 36 (33.6) | 10 (9.3) | 53 (49.5) | 107 (100.0) | |||
| Widow/widower | 0 (0.0) | 1 (25.0) | 0 (0.0) | 3 (75.0) | 4 (100.0) | |||
| Age group | ||||||||
| ≤19 years | 1 (5.6) | 7 (38.9) | 1 (5.6%) | 9 (50.0) | 18 (100.0) | 9.731 | 12 | 0.640 |
| 20–29 years | 8 (10.0) | 25 (31.3) | 8 (10.0) | 39 (48.8) | 80 (100.0) | |||
| 30–39 years | 4 (8.2) | 19 (38.8) | 2 (4.1) | 24 (49.0) | 49 (100.0) | |||
| 40–49 years | 0 (0.0) | 11 (32.4) | 1 (2.9) | 22 (64.7) | 34 (100.0) | |||
| 50 and above | 2 (7.7) | 12 (46.2) | 1 (3.8) | 11 (42.3) | 26 (100.0) | |||
| Education | ||||||||
| Primary schooling | 1 (12.5) | 4 (50.0) | 0 (0.0) | 3 (37.5) | 8 (100.0) | 12.056 | 15 | 0.675 |
| Secondary | 2 (4.0) | 21 (42.0) | 2 (4.0) | 25 (50.0) | 50 (100.0) | |||
| Higher secondary | 7 (13.2) | 19 (35.8) | 3 (5.7) | 24 (45.3) | 53 (100.0) | |||
| ITI | 1 (12.5) | 4 (50.0) | 0 (0.0) | 3 (37.5) | 8 (100.0) | |||
| Diploma | 0 (0.0) | 4 (28.6) | 1 (7.1) | 9 (64.3) | 14 (100.0) | |||
| Graduate | 4 (5.4) | 22 (29.7) | 7 (9.5) | 41 (55.4) | 74 (100.0) | |||
| Occupation | ||||||||
| Employed | 5 (8.6) | 14 (24.1) | 3 (5.2) | 36 (62.1) | 58 (100.0) | 18.773 | 16 | 0.094 |
| Unemployed | 5 (6.0) | 33 (39.8) | 4 (4.8) | 41 (49.4) | 83 (100.0) | |||
| Home maker | 1 (2.9) | 18 (51.4) | 1 (2.9) | 15 (42.9) | 35 (100.0) | |||
| Student | 4 (14.3) | 8 (28.6) | 5 (17.9) | 11 (39.3) | 28 (100.0) | |||
| Retired | 0 (0.0) | 1 (33.3) | 0 (0.0) | 2 (66.7) | 3 (100.0) | |||
| Socio economic status | ||||||||
| Upper class | 0 (0.0) | 2 (50.0) | 0 (0.0) | 2 (50.0) | 4 (100.0) | 11.259 | 12 | 0.507 |
| Upper middle class | 2 (11.1) | 5 (27.8) | 0 (0.0) | 11 (61.1) | 18 (100.0) | |||
| Middle class | 8 (9.2) | 26 (29.9) | 7 (8.0) | 46 (52.9) | 87 (100.0) | |||
| Lower middle class | 2 (4.9) | 17 (41.5) | 5 (12.2) | 17 (41.5) | 18 (100.0) | |||
| Lower class | 3 (5.3) | 24 (42.1) | 1 (1.8) | 29 (50.9) | 57 (100.0) |
Associations between psychiatric diagnosis and lunar phase
Major mental illness was categorized to find any association between psychiatric diagnosis and lunar phases. The result shows that at ±3 days around new moon 54% of the patients were with BPAD mania, 53% with Schizophrenia, and 40.5% with ATPD. It was also high at ±3 days around full moon in ATPD with 50%, 37% in Schizophrenia and 29% in BPAD mania. The chi-square test shows that there was no significant association between different lunar phases and psychiatric diagnosis (P = 0.399) [Table 2].
| Diagnosis | Full moon n (%) |
Full moon±3 days n (%) |
New moon n (%) |
New moon±3 days n (%) |
Total n (%) |
χ2 | df | P-value |
|---|---|---|---|---|---|---|---|---|
| Schizophrenia | 5 (6.8) | 27 (36.5) | 3 (4.1) | 39 (52.7) | 74 (100.0) | 9.43 | 9 | 0.399 |
| BPAD Mania | 9 (9.9) | 26 (28.6) | 7 (7.7) | 49 (53.8) | 91 (100.0) | |||
| ATPD | 1 (2.3) | 21 (50.0) | 3 (7.2) | 17 (40.5) | 42 (100.0) |
Associations between duration admissions of patients with the lunar phase
The duration of admission of patients in the hospital according to the lunar phases was analysed and found that the average duration was high among patients admitted during 3 days around new moon (10.44 days), followed by full moon day (9.87 days), new moon (9.54 days) and 3days around full moon (9.43 days). Analysis of variance test was applied to find the differences in duration of admission at different lunar phases and found that there was no significant difference in mean duration (P = 0.704) [Table 3].
| Lunar phase | n | Mean | Std. deviation | 95% Confidence interval for the mean | P-value | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Full moon | 15 | 9.87 | 4.42 | 7.42 | 12.32 | 0.704 |
| Full moon±3 days | 74 | 9.43 | 5.55 | 8.15 | 10.72 | |
| New moon | 13 | 9.54 | 5.87 | 5.99 | 13.08 | |
| New moon±3 days | 105 | 10.44 | 6.07 | 9.26 | 11.61 | |
| Total | 207 | 9.98 | 5.75 | 9.19 | 10.77 | |
Associations of symptom exacerbation of major mental illness with different lunar phases
The presence of symptoms of exacerbation of mental with different lunar phases was analyzed and found that it was high with 46% among patients affected during the new moon, followed by 3 days around new moon (10.5%), 3 days around full moon (6.8% and full moon (6.7%). The chi-square test shows that there was a significant association between symptom exacerbation of major mental illness and different lunar phases (P = 0.001) [Table 4].
| Lunar phase | Exacerbation present n (%) |
Exacerbation absent n (%) |
Total n (%) |
χ2 | df | P-value |
|---|---|---|---|---|---|---|
| Full moon | 1 (6.7) | 14 (93.3) | 15 (100.0) | 17.927 | 3 | 0.001 |
| Full moon±3 days | 5 (6.8) | 69 (93.2) | 74 (100.0) | |||
| New moon | 6 (46.2) | 7 (53.8) | 13 (100.0) | |||
| New moon±3 days | 11 (10.5) | 94 (89.5) | 105 (100.0) | |||
| Total | 23 (11.1) | 184 (88.9) | 207 (100.0) |
Associations between chemical restraints and lunar phases
The injection was given to 64% of patients belonging to ± 3 days around full moon and 47% in full moon period. It was 44% in ± 3 days around new moon and 39% in new moon period. The Chi-square test shows that there was a significant association present between chemical restraints and lunar phases (P = 0.001) [Table 5].
| Lunar phase | Injection given n (%) |
Injection not given n (%) |
Total n (%) |
χ2 | df | P-value |
|---|---|---|---|---|---|---|
| Full moon | 7 (46.7) | 8 (53.3) | 15 (100.0) | 17.927 | 3 | 0.001 |
| Full moon±3 days | 47 (63.5) | 27 (36.5) | 74 (100.0) | |||
| New moon | 5 (38.5) | 8 (61.5) | 13 (100.0) | |||
| New moon±3 days | 46 (43.8) | 59 (56.2) | 105 (100.0) | |||
| Total | 105 (50.7) | 102 (49.3) | 207 (100.0) |
Association between caregiver belief on symptom worsening and lunar phase
Caregiver belief on symptom worsening was high at new moon 6(46.2%) followed by ±3days around new moon 19 (23.5%), ±3 days around full moon 12 (18.5%), and full moon (13.3%). The chi-square test shows that there was no association between caregiver belief on worsening of symptoms with lunar phases (P = 0.135) [Table 6].
| Lunar phase | Caregiver belief on symptom worsening | χ2 | df | P-value | ||
|---|---|---|---|---|---|---|
| Yes n (%) | No n (%) | Total n (%) | ||||
| Full moon | 2 (13.3) | 13 (86.7) | 15 (100.0) | 5.559 | 3 | 0.135 |
| Full moon±3 days | 12 (18.5) | 53 (81.5) | 65 (100.0) | |||
| New moon | 6 (46.2) | 7 (53.8) | 13 (100.0) | |||
| New moon±3 days | 19 (23.5) | 62 (76.5) | 81 (100.0) | |||
| Total | 39 (22.4) | 135 (77.6) | 174 (100.0) | |||
Symptom worsening noted caregiver during lunar phases
From 207 participants we were able to contact and verify 174 participants through telephone to assess caregiver belief on symptom worsening during the lunar phase and to get details about whether they noted any symptom worsening during full moon and new moon.
Symptom worsening noted by caregiver during lunar phases was high with 46.2% during new moon phase, 27.2% in ± 3 days around new moon, 18.5% in ±3 days around full moon and 13.3% in full moon days. The chi-square test shows that there was no association between symptom worsening noted by caregiver and the lunar phase (P = 0.114). Lunar phases had no effect on worsening of mental illness as believed by caregiver [Table 7].
| Lunar phase | Symptom worsening noted by care giver | χ2 | df | P-value | ||
|---|---|---|---|---|---|---|
| Yes n (%) | No n (%) | Total n (%) | ||||
| Full moon | 2 (13.3) | 13 (86.7) | 15 (100.0) | 5.945 | 3 | 0.114 |
| Full moon±3 days | 12 (18.5) | 53 (81.5) | 65 (100.0) | |||
| New moon | 6 (46.2) | 7 (53.8) | 13 (100.0) | |||
| New moon±3 days | 22 (27.2) | 59 (72.8) | 81 (100.0) | |||
| Total | 42 (24.1) | 132 (75.9) | 174 (100.0) | |||
Comparison of cases during fullmoon, new moon and rest of the days
Graph 1 shows that the black line drawn in center denotes the average admission of cases and the line marked in the red line denotes the admission of patients during phases of moon the highest peak of admission was noted two days earlier than the new moon. The graph also reveals that the admission of the patient is more during different phases of moon compare to other days.
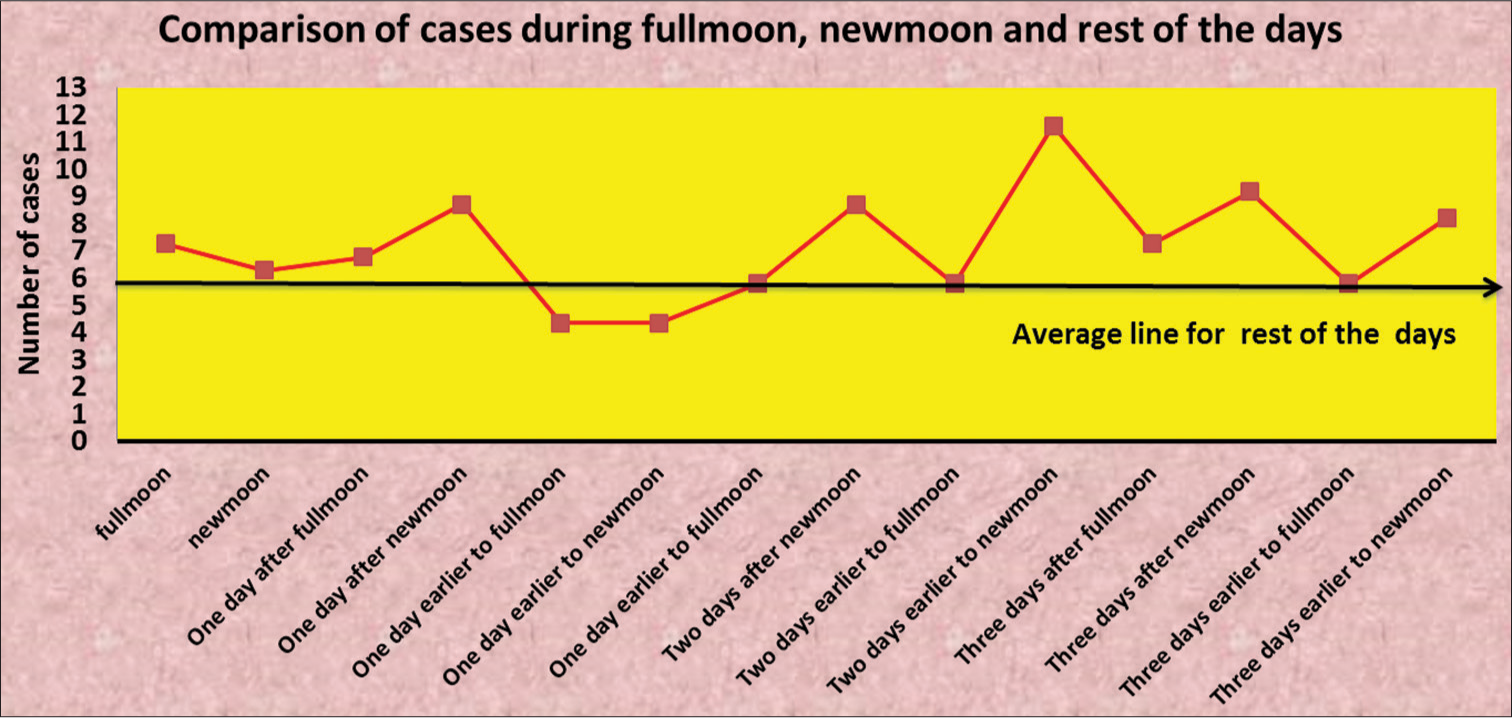
- Comparison of cases during full moon, new moon and rest of the days.
DISCUSSION
A retrospective study was conducted to evaluate the association of lunar phases with mental illness such as schizophrenia, BPAD mania, and ATPD. The relationship between the association of lunar phases and mental illness is ambiguous. The individual variables such as gender, age, education, and income levels were are all had no noteworthy association with lunar phases in this study. A study done by Kazemi-Bajestani et al., which also shows there is no correlation between the lunar cycle and gender which is in concordance with this study.[11]
In our study, psychiatric patients admitted during ± 3 days around the new moon were highest with 50% and 6.3% in new moon admission which is the lowest. The results show there is statistical significance present between admission and lunar phases (P = 0.001). A similar study done by Gorvin and Roberts, there is no significant presence between psychiatric admission and lunar phases and one another study done by Mclay et al., and shows there was no association between admission and lunar phase.[12,13] Another study done by Maslov also reveals there is no relationship between admission and the lunar cycle (P = 0.438).[14]
In our study, the psychiatric patient restrained using chemical restraints during different lunar phases where highest among patients admitted during ±3 days during full moon and second highest with patient admitted during full moon with 46.7% and lowest during new moon period at 38.5%. The result shows there was a significant association between chemical restraint and lunar phases with (P < 0.001). The chemical restraint depends on the doctor’s decision. A similar study done by Mittal et al., their results shows there is a positive significant presence for phases of moon and chemical restraint (P < 0.0008) which is in concordance with this study.[9] The chemical restraint depends upon the doctor’s decision. Another study done by Kazemi-Bajestani et al. shows there is no correlation between chemical restraint and the lunar cycle (P = 0.130).[11]
Patient admitted with schizophrenia during different lunar phases was 35.7%, 44% were diagnosed with BPAD mania and 20.3% were diagnosed with ATPD in this study. The result shows there is no significant association between diagnosis and the lunar phase. A similar study done by Francis et al., reveals there is no association between psychiatric diagnosis and lunar phases.[1] Another study done by Kakunje also reveals that there is no statistical significance between psychiatric diagnosis and lunar phases.[15]
The mean duration of admission was highest for patients admitted during ± 3 days during new moon with 10.44 and lowest for patients admitted during ± 3 days during full moon with 9.43 in this study. The results show there is no association between duration of admission and lunar phases (P = 0.704). A similar study done by Gupta et al., shows there is no relationship between length of stay and lunar cycle which is in concordance with this study.[6]
Symptom exacerbation noted by caregiver during the lunar cycle was highest during the new moon at 46.2% and lowest with full moon at 13.3% and there is no correlation between symptom exacerbation noted by caregiver and lunar phases (P = 0.114). Caregiver belief on symptom worsening and lunar phase was highest with new moon and lowest with the full moon and there is no significant association between caregiver belief on symptom worsening and the lunar phase (P = 0.135) this implies there is the caregiver belief o lunar cycle do not have an impact on out-come of symptom worsening during full moon and new moon.
Symptom exacerbation of psychiatric illness was highest during new moon period with 46.2% and least during full moon period with 6.7% in this study. The results show there is statistical significance present between symptom exacerbation and lunar phases. A similar study done by Wang et al., from China in 13,607 patients admitted to psychiatric hospital from 2012 to 2017 revealed psychiatric symptoms in schizophrenia patient aggravated more during the full moon and stable during new moon which is opposite to our study that is symptom exacerbation was more during new moon day than during full moon day in our study.[2]
The comparison of cases during full moon, new moon and the rest of the days, the peak admission was noted during different phases of moon. The peak of admission during phases of moon was highest with 11 during two days earlier to the new moon compared to the average admission was 5 during the rest of the days. The lowest admission was noted one day earlier to full moon and new moon. Most of the admission was higher during different phases of moon compared with the rest of the days. This reveals there is a relationship between symptom worsening and different phases of the moon.
The limitations of the current study are in the retrospective nature of the study design. Large studies analyzing lunar pattern-based associations with specific mental disorders prospectively may add more value.
CONCLUSION
The exacerbation of mental illness, chemical restraints, and admission was associated significantly with lunar patterns in the study population. The rest of the sociodemographic factors, duration of admission, caregiver belief, and symptom worsening noted by caregiver were all not associated with mental illness during lunar phases which are in line with most reported literature in this area.
Acknowledgment
We acknowledge the support provided by the Medical records department in helping in retrieving the medical records for this study.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Psychiatric presentations during all 4 phases of the lunar cycle. Adv Mind Body Med. 2017;31:4-7.
- [Google Scholar]
- Lunar cycle and psychiatric hospital admissions for schizophrenia: New findings from Henan province, China. Chronobiol Int. 2020;37:438-49.
- [CrossRef] [PubMed] [Google Scholar]
- Admission to intensive care for parasuicide by self-poisoning: Variation by time cycles, climate and the lunar cycle. Psychiatry Res. 2008;161:177-84.
- [CrossRef] [PubMed] [Google Scholar]
- Much ado about the full moon: A meta-analysis of lunar-lunacy research. Psychol Bull. 2015;97:286-306.
- [CrossRef] [Google Scholar]
- Is it the moon? Effects of the lunar cycle on psychiatric admissions, discharges and length of stay. Swiss Med Wkly. 2019;149:w20070.
- [CrossRef] [PubMed] [Google Scholar]
- A link between lunar phase and medically unexplained stroke symptoms: An unearthly influence? J Psychosom Res. 2008;65:131-3.
- [CrossRef] [PubMed] [Google Scholar]
- Madness and the moon: The lunar cycle and psychopathology. German J Psychiatry. 2006;9:123-7.
- [Google Scholar]
- Does lunar synodic cycle affect the rates of psychiatric hospitalizations and sentinel events? Chronobiol Int. 2021;38:360-6.
- [CrossRef] [PubMed] [Google Scholar]
- Synodic lunar phases and suicide: Based on 2605 suicides over 23 years, a full moon peak is apparent in premenopausal women from northern Finland. Mol Psychiatry. 2021;26:5071-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lunar phase cycle and psychiatric hospital emergency visits, inpatient admissions and aggressive behavior. Asian J Psychiatry. 2011;4:45-50.
- [CrossRef] [PubMed] [Google Scholar]
- Lunar phases and psychiatric hospital admissions. Psychol Rep. 1994;75(3 Suppl):1435-40.
- [CrossRef] [PubMed] [Google Scholar]
- No effect of lunar cycle on psychiatric admissions or emergency evaluations. Mil Med. 2006;171:1239-42.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of moon phases on the frequency of admissions to a psychiatric hospital. Izv Atmos Ocean Phys. 2002;58:708-12.
- [CrossRef] [Google Scholar]
- Lunar effect or Transylvania effect: The moon and mind connection. Indian J Private Psychiatry. 2020;14:48.
- [CrossRef] [Google Scholar]