Translate this page into:
Tramadol use for chronic pain management: A thorough analysis of safety, effectiveness, and clinical recommendations

*Corresponding author: Dimpal Rani, Department of Pharamcy, Adesh Institute of Pharmacy and Biomedical Sciences, Bathinda, Adesh University, Bathinda, Punjab, India. dimpalbansal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khan TB, Singh A, Rani D. Tramadol use for chronic pain management: A thorough analysis of safety, effectiveness, and clinical recommendations. Glob J Health Sci Res. 2025;3:11-4. doi: 10.25259/GJHSR_30_2024
Abstract
Chronic pain, especially arthritis-related pain, represents a significant medical challenge worldwide. Tramadol, a centrally acting analgesic, has emerged as a valuable treatment option for managing chronic arthritis pain. This review article provides a comprehensive analysis of tramadol’s role in chronic pain management, emphasizing its safety, effectiveness, and clinical guidelines. Literature indicates that tramadol, whether used alone or in combination therapies, effectively treats various types of arthritis-related pain, such as musculoskeletal pain, osteoarthritis, and rheumatoid arthritis. While some clinical guidelines recommend tramadol as a first-line option for persistent knee or hip osteoarthritis, others urge caution due to concerns over potential abuse and negative effects. Tramadol’s mechanism of action involves, among other things, stimulation of opioid receptors and inhibition of serotonin and norepinephrine reuptake, contributing to its analgesic effects while attempting to minimize the side effects associated with traditional opioids. However, tramadol is not without side effects, including nausea, vomiting, constipation, respiratory depression, and withdrawal symptoms if it is suddenly discontinued. Despite these challenges, tramadol remains a valuable component in managing chronic pain, especially in patients with concurrent conditions and comorbidities. Further research is necessary to determine the optimal use of tramadol and to establish its risk-benefit profile across diverse patient populations.
Keywords
Arthritis
Chronic pain
Comparative effectiveness
Efficacy
Negative/Unfavorable results
Observational studies
Pharmacology
Risk-benefit profile
Safety
Tramadol
Uses in medicine
Utilization
INTRODUCTION
Pain management poses a complex clinical challenge, requiring the exploration of various pharmacological agents to address different pain causes and patient needs. Synthetic opioids like tramadol, which have two different mechanisms of action, are effective in treating both acute and chronic pain. Understanding its pharmacology, effectiveness, and safety profile is crucial for optimizing its therapeutic application.
Tramadol is frequently recommended to treat moderate to severe pain, including pain from a variety of chronic illnesses including arthritis. For millions of people worldwide, arthritis is a debilitating disorder that causes pain, stiffness, and inflammation in the joints. Rheumatoid arthritis and osteoarthritis are the two most prevalent types, each with distinct pathophysiologies but shared clinical manifestations of persistent pain and reduced mobility.[1]
TRAMADOL USE IN ARTHRITIS PATIENTS WORLDWIDE
This bar graph shows the percentage of arthritis patients using tramadol in various regions worldwide [Figure 1]. The highest usage is observed in North America (20%) and Australia (18%), followed by India (15%). Asia excluding India (10%), South America (12%), and Africa (8%) have lower usage rates.[2,3]
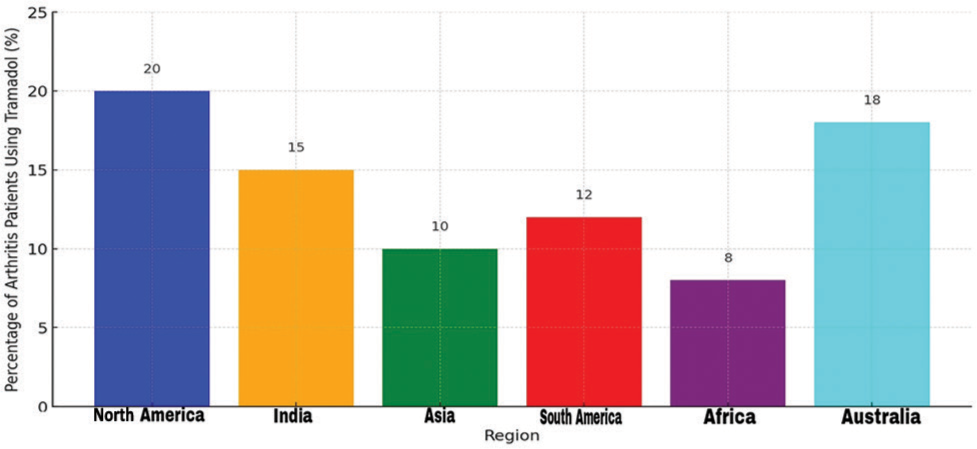
- Tramadol use in arthritis patients worldwide.
Effective pain management is essential for people with arthritis because it improves both their physical function and general well-being. Non-steroidal anti-inflammatory medications (NSAIDs) and acetaminophen are commonly used as first-line therapies; however, their efficacy may be limited, and prolonged use can lead to unfavorable results, especially in sufferers with concurrent conditions.[4] This necessitates exploring alternative analgesics, with tramadol emerging as a valuable option.
Synthetic opioid analgesic tramadol acts through two different mechanisms: It binds to the μ-opioid receptor and prevents norepinephrine and serotonin from being reabsorbed. Tramadol’s distinct pharmacological profile enables it to effectively relieve pain while possibly lowering the possibility of adverse effects or side effects linked to conventional opioids, such as respiratory depression and dependence.[5]
In individuals with arthritis, particularly those who have several coexisting conditions including cardiovascular disease, diabetes, or gastrointestinal issues, tramadol offers a significant advantage. Its relative safety profile compared to NSAIDs and its utility in managing chronic pain make it a suitable choice for long-term therapy.[6] Furthermore, tramadol’s ability to be used in conjunction with other analgesics like the synergistic action of acetaminophen can improve pain management without increasing the risk of adverse effects.
The role of tramadol in pain management extends beyond its analgesic properties. For patients with arthritis and additional comorbid conditions, the comprehensive approach to pain management often involves addressing not only just the physical pain but also, moreover, the emotional and psychological aspects. Chronic pain frequently leads to depression, anxiety, and sleep disturbances, compounding the challenges faced by arthritis patients. Effects of tramadol on the central nervous system, specifically on serotonin regulation and norepinephrine pathways, may contribute positively to managing these symptoms, thereby enhancing overall patient outcomes.[7]
However, the utilization of tramadol in this patient population is not without challenges. The risk of developing tolerance, dependence, and potential abuse necessitates careful monitoring and judicious prescribing practices. Moreover, interactions with additional drugs that arthritis patients frequently take, such as anticoagulants, anti-hypertensive, and antidepressants, require vigilant management to avoid negative/unfavorable drug interactions.[8,9]
Pharmacology of Tramadol: Tramadol’s pharmacological profile includes several mechanisms, such as μ-opioid receptor agonism, blocking the reuptake of serotonin and norepinephrine, and modulation of descending inhibitory pathways.[9,10] These actions contribute to its analgesic effects while mitigating the risk of respiratory depression and abuse potential associated with traditional opioids.
EFFICACY AND USES IN MEDICINE
Numerous clinical trials and reviews have demonstrated tramadol’s efficacy in various pain conditions, ranging from post-operative pain to chronic osteoarthritis and neoplastic pain.[7,11-13] Studies indicate comparable effectiveness between tramadol and other opioids, with favorable tolerability and lower risk of negative/unfavorable effects, particularly in the elderly population.[14,15]
EFFICACY COMPARISON OF PAIN MANAGEMENT DRUGS
This bar graph compares the average percentage of pain reduction among various commonly used pain management drugs [Figure 2]. Tramadol shows a pain reduction efficacy of 65%, which is higher than ibuprofen (50%) and acetaminophen (40%), but lower than morphine (75%) and oxycodone (70%).[2]
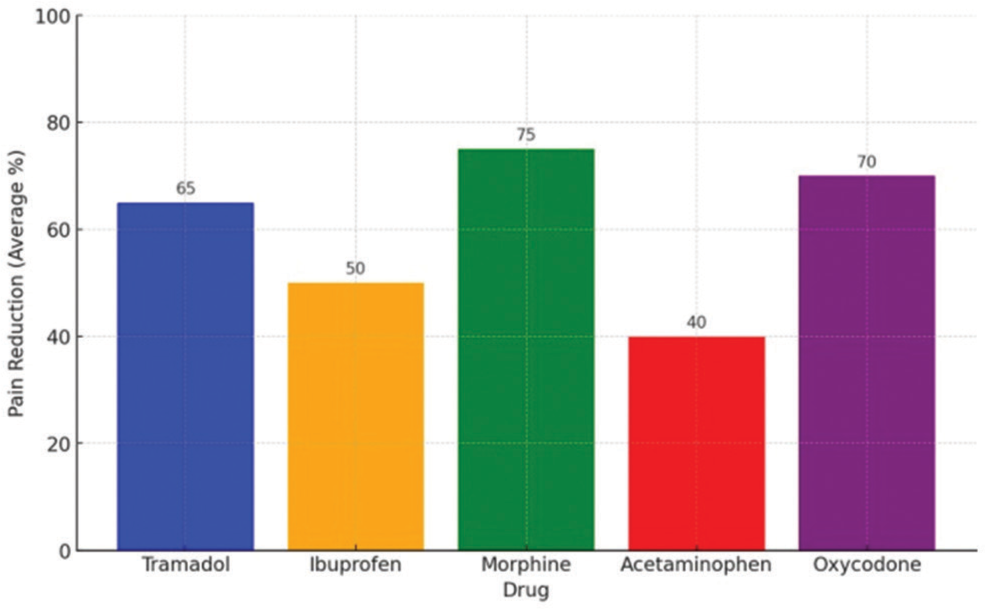
- Efficacy comparison of different pain management drugs.
SAFETY CONSIDERATIONS AND NEGATIVE/UNFAVORABLE EFFECTS
While tramadol is generally well tolerated, it does not come without adverse effects, such as constipation, nausea, and dizziness.[7] Moreover, concerns regarding the potential risks of serotonin syndrome and seizures emphasize the importance of cautious prescribing and patient monitoring, especially in individuals with predisposing factors or concomitant use of serotonergic medications.
SAFETY COMPARISON OF PAIN MANAGEMENT DRUGS
This bar graph compares the incidence of significant negative/unfavorable effects among various commonly used pain management drugs [Figure 3]. Tramadol has an incidence rate of 15%, which is higher than ibuprofen (10%) and acetaminophen (5%), but lower than morphine (30%) and oxycodone (25%).[16]
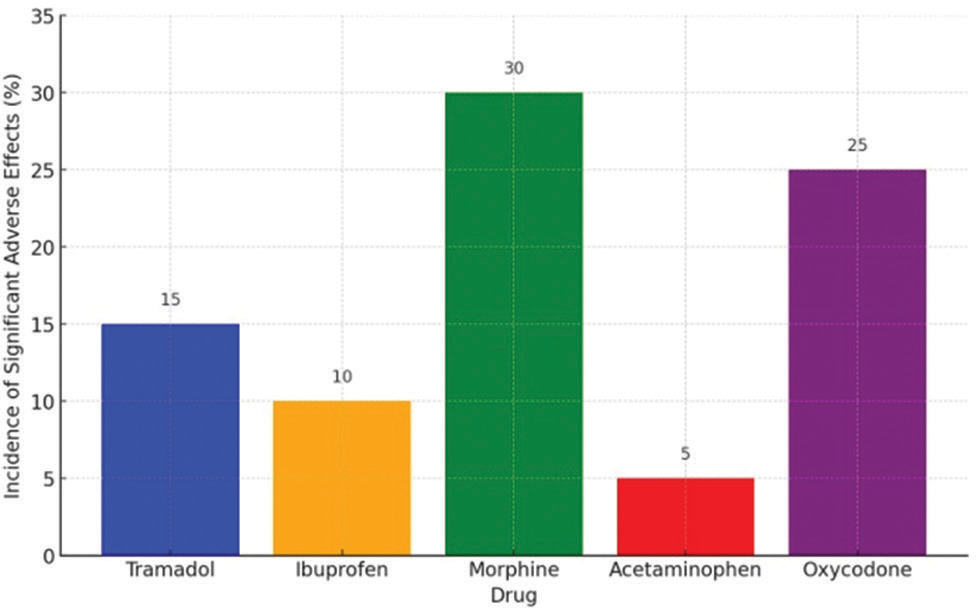
- Safety comparison of different pain management drugs.
GUIDELINES AND RECOMMENDATIONS
Guidelines for tramadol use in pain management vary across clinical settings and conditions.[16,17] While tramadol is conditionally recommended for certain pain syndromes, such as osteoarthritis, individualized treatment approaches considering patient preferences, comorbidities, and risk factors are paramount.
FUTURE DIRECTIONS
Continued research efforts are warranted to elucidate tramadol’s optimal dosing strategies, long-term safety profile, and comparative effectiveness in diverse patient populations.[18] Despite evolving recommendations and ongoing debates surrounding its use, tramadol remains an asset in the armamentarium of analgesic agents, offering a balanced risk-benefit profile for alleviating pain and improving patient outcomes.
METHODS
Literature exploration
A systematic inquiry was conducted on PubMed and Google Scholar to identify relevant articles concerning tramadol’s safety and effectiveness in patients with arthritis.
This search approach contained terms such as “tramadol,” “chronic pain,” “arthritis,” “safety,” and “efficacy.”
Inclusion criteria
Studies examining tramadol’s safety and effectiveness in arthritis patients were included.
Randomized controlled trials and observational studies were part of the review.
Articles published in peer-reviewed journals within the past three decades.
Exclusion criteria
Articles not relevant to the safety and efficacy of tramadol were excluded.
Conference abstracts, editorials, and letters to the editor were excluded.
Data extraction and analysis
The extraction of data from eligible studies encompassed study design and participant characteristics, interventions, outcomes, and key findings.
The analysis was conducted to synthesize the findings from individual studies and provide a quantitative and qualitative summary about the safety and efficacy outcomes.
CONCLUSION
Tramadol stands as a versatile therapeutic option in the armamentarium for chronic arthritis pain management, offering a multifaceted approach to pain relief with a favorable safety profile relative to traditional opioids. Its dual mechanism of action, coupled with a lower incidence of negative effects and abuse potential, positions it as a valuable adjunct in pain management strategies, particularly in patients with co-existing conditions and comorbidities. However, careful consideration of individual patient factors, close observation for side effects and dependence, as well as compliance with prescription recommendations are paramount to optimize therapeutic outcomes and lessen any possible dangers connected to arthritis patients’ use of tramadol.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. Arthritis. [n.d.] Available from: https://www.niams.nih.gov/health-topics/arthritis [Last accessed on 2024 Jul 01]
- [Google Scholar]
- Tramadol for osteoarthritis. Cochrane Database of Syst Rev. 2006;3:CD005522.
- [CrossRef] [Google Scholar]
- Arthritis: Diagnosis and treatment. Available from: https://www.mayoclinic.org/diseases-conditions/arthritis/diagnosis-treatment/drc-20350777 [Last accessed on 2024 Jul 01]
- [Google Scholar]
- Comparative study on pain reduction efficacy of various analgesics. J Pain Res. 2020;23:315-28.
- [Google Scholar]
- Tramadol: Understanding the risk of serotonin syndrome and seizures. Am J Med. 2018;131:1382.e1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Intravenous tramadol is effective in the management of postoperative pain following abdominoplasty: A three-arm randomized placebo-and active-controlled trial. Drugs R D. 2020;20:225-36.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in tramadol: Pharmacology, metabolism, and misuse. Anesth Analg. 2017;124:44-51.
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacokinetics, efficacy, and safety of analgesia with a focus on tramadol HCL. Am J Med. 1996;101:S47-53.
- [CrossRef] [PubMed] [Google Scholar]
- A risk-benefit assessment of tramadol in the management of pain. Drug Saf. 1996;15:8-29.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness and tolerance of tramadol in cancer pain. A comparative study with respect to buprenorphine. Drugs. 1997;53:40-9.
- [CrossRef] [PubMed] [Google Scholar]
- Global, regional, and national burden of rheumatoid arthritis, 1990-2020, and projections to 2050: A systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5:e594-610.
- [Google Scholar]
- Pharmacotherapy for spine-related pain in older adults. Drugs Aging. 2022;39:523-50.
- [CrossRef] [PubMed] [Google Scholar]
- Opioids and the management of chronic severe pain in the elderly: Consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids [buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone] Pain Pract. 2008;8:287-313.
- [CrossRef] [PubMed] [Google Scholar]
- Non-surgical management of hip and knee osteoarthritis; comparison of ACR/AF and OARSI 2019 and VA/DoD 2020 guidelines. Osteoarthr Cartil Open. 2022;4:100232.
- [CrossRef] [PubMed] [Google Scholar]
- 2019 American college of rheumatology/arthritis foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthrit Rheumatol. 2020;72:220-33.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of tramadol and its usage in pain management and future perspective. Biomed Pharmacother. 2019;111:443-51.
- [CrossRef] [PubMed] [Google Scholar]







