Translate this page into:
Why should we pay attention to occupational history? Two case reports

*Corresponding author: Asuman Aslan Kara, Department of Occupational Disease, Ankara Atatürk Sanatorium Training and Research Hospital, Ankara, Turkey. drasuaslan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aslan Kara A, Sarı G, Koyuncu A, Şimşek C. Why should we pay attention to occupational history? Two case reports Glob J Health Sci Res. 2025;3:43-5. doi: 10.25259/GJHSR_38_2024
Abstract
The diagnosis of occupational lung diseases requires a high level of suspicion and a comprehensive occupational history. Neglecting this can lead to delayed diagnosis and inappropriate management. In advanced stages of pneumoconiosis, progressive massive fibrosis (PMF) masses may develop. Distinguishing between PMF and lung cancer in advanced pneumoconiosis cases can be difficult. Insufficient questioning about occupational history in these cases may lead to unnecessary invasive procedures and worsen existing pneumoconiosis. This study aimed to highlight the significance of obtaining a thorough occupational history in diagnosing and differentiating occupational diseases. Two cases are presented where patients were admitted to our clinic after undergoing invasive procedures for suspected interstitial lung disease and lung cancer at another institution. A detailed occupational history combined with characteristic radiological findings diagnosed with pneumoconiosis. In patients with pneumoconiosis, it is of great importance to establish an exposure-causality relationship with a detailed occupational history.
Keywords
Lung malignancy
Occupational history
Pneumoconiosis
Progressive massive fibrosis
INTRODUCTION
The diagnosis of occupational lung diseases requires a high level of suspicion and a comprehensive occupational history. Neglecting this can lead to delayed diagnosis and inappropriate management. In advanced stages of pneumoconiosis, progressive massive fibrosis (PMF) masses may develop. These masses are formed by the merging of fibrotic foci and can cause structural damage to the lungs. Distinguishing between PMF and lung cancer in advanced pneumoconiosis cases can be difficult. Insufficient questioning about occupational history in these cases may lead to unnecessary invasive procedures and worsen existing pneumoconiosis.
The purpose of presenting these cases is to highlight the significance of obtaining a thorough occupational history in diagnosing and differentiating occupational diseases. In addition, it aims to discuss the factors to be taken into account when deciding on the need for invasive procedures.
CASE SERIES
Case 1
A 39-year-old male patient, admitted to an external center with back pain, and underwent a fiberoptic bronchoscopy (FOB) biopsy with the preliminary diagnosis of respiratory bronchiolitis-interstitial lung disease (RB-ILD). Subsequently, a wedge biopsy of the right lung was performed, revealing pigments containing Prussian blue in the macrophages. The patient was then referred to us after providing his occupational history. He had no active complaints during his visit. With a 30-pack-year smoking history, the patient had worked as a welder for 15 years and had a family history of lung cancer in his father. There was no history of pet feeding. Pulmonary function tests and laboratory values were normal.
Posteroanterior chest x-ray (PA-CXR) showed ground-glass dense nodular densities in the upper and middle zones bilaterally [Figure 1a]. High-resolution chest tomography (HRCT) revealed diffuse millimetric nodular-sentriacinar ground-glass infiltrations in the upper-middle zones of both lungs with a tendency to merge [Figure 1b]. An occupational disease specialist diagnosed stage 2 silicosis with International Labor Organization (ILO) reading q/q 2/1.
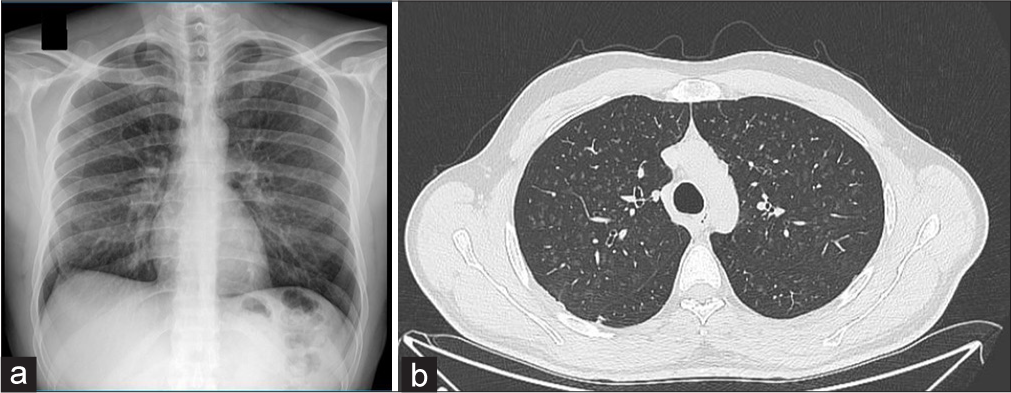
- (a) Bilateral upper and middle Zon ground-glass dense nodular densities and (b) diffuse millimetric nodular-sentriacinar ground-glass infiltrations.
Case 2
Our patient, a 79-year-old male with no known history of chronic disease, presented to an external center with back pain and underwent Endobronchial Ultrasound followed by FOB-Transbronchial needle aspiration with the preliminary diagnoses of lung cancer and metastasis. However, no definitive diagnosis was obtained from the biopsy materials. The patient was subsequently referred to us, with no active complaints at the time of his visit. It was revealed that the patient had been working as a welder and iron grinder for 67 years, with a smoking history of 104 pack-years and a history of cerebrovascular disease. Physical examination showed decreased respiratory sounds, moderate obstruction in the pulmonary function tests (Forced expiratory volume/forced vital capacity (FEV 1/FVC) 62%, FEV 1% 74), normal diffusion tests, and laboratory values. PAAC Graphy showed bilateral nodular density increases above 3 mm and bilateral opacity increases [Figure 2a]. HRCT revealed mediastinal and hilar enlarged lymph nodes with a narrow transverse dimension of 12 mm and nodular infiltrations, the largest of which was 12 mm in diameter with a partially recessed contour, emphysematous changes in both lungs [Figure 2b]. The patient was diagnosed with complicated pneumoconiosis with ILO reading r/q 2/2, A2 by an occupational disease specialist.
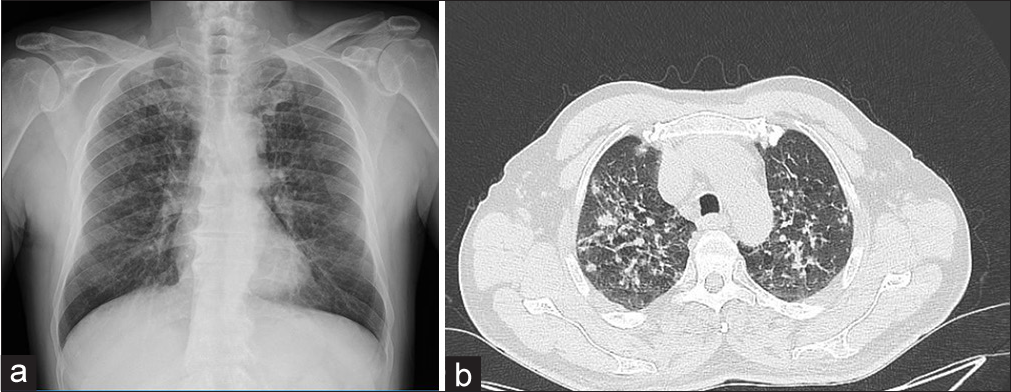
- (a) Bilateral nodular densities and opacity increases, (b) Nodular infiltrations, with a partially recessed contour, emphysematous changes.
DISCUSSION
In respiratory system diseases, as in all systems, history is crucial. In occupational respiratory system diseases, exposure can be revealed with a detailed occupational history. Silicosis is the most common occupational lung disease and is an irreversible restrictive lung disease, characterized by inflammation and pulmonary fibrosis. It is an incurable, preventable disease with serious morbidity and mortality. Prevention, screening, timely diagnosis, avoidance of trigger factors, and treatment of complications are vital.
Silicosis occurs in acute, accelerated, and chronic forms. Chronic silicosis is the most common form and typically develops 10–30 years after prolonged exposure to low concentrations.[1,2] Radiographic findings are used to distinguish between simple and complicated chronic silicosis[3] Chronic simple silicosis is characterized by well-defined nodules <10 mm in diameter, usually in the upper lobes, with perilymphatic distribution and may be accompanied by mediastinal and hilar lymphadenopathy. Complicated chronic silicosis or PMF presents as calcified, bilateral, symmetrical, conglomerate masses with irregular edges, larger than 1 cm in diameter, and associated with parascatricial emphysema.[4-6] Patients with PMF often develop respiratory failure due to lung tissue damage, leading to impaired lung function, pulmonary hypertension, and cor pulmonale. The radiographic opacities of silicosis patients often resemble those of other lung diseases such as sarcoidosis, tuberculosis, or malignancy.[6] There is no specific laboratory test for diagnosis, it relies on compatible exposure history and consistent radiological features and requires the exclusion of alternative diagnoses. A detailed occupational history is the cornerstone of a correct diagnosis, as it brings us closer to the correct diagnosis. Pay attention to the clinical history, including occupational exposure, is vital to exclude more common diseases and arrive at an accurate diagnosis.[7] In summary, a comprehensive occupational history is essential for diagnosing of occupational diseases. Although silicosis cannot be cured, it can be prevented by controlling exposure.[3]
Since there is no cure for silicosis, timely and accurate diagnosis is crucial to prevent further exposure and avoid unnecessary invasive diagnostic procedures and potentially harmful treatment. Even in cases of atypical appearance or unusual presentation, invasive procedures cannot replace the need for a detailed occupational history.[8] Invasive procedures silicosis patients are considered hazardous as they can worsen the patient’s condition, negatively impacting their quality of life and mortality.[9,10] Diagnosing PMF in the presence of typical radiology findings is not difficult.[11] Therefore, noninvasive imaging diagnosis is essential for differential diagnosis.[12]
In the first case, bronchoscopic biopsy and surgical biopsy were performed with a preliminary diagnosis of RB-ILD due to insufficient questioning about occupational history. In the second case with typical PMF radiology, invasive procedures such as bronchoscopic biopsy and lymph node biopsy were performed with the preliminary diagnosis of lung cancer. If regular screening programs had been implemented in the workplace in this case, the diagnosis of silicosis may have been possible at an early stage and could have slowed the progression of pulmonary fibrosis. These cases highlight the importance of taking a detailed occupational history to avoid invasive procedures that could worsen prognosis and quality of life. They also emphasize the benefits of regular workplace screening and early diagnosis in slowing down disease progression.
CONCLUSION
Establishing an exposure-causality relationship through a detailed occupational history is crucial for patients with pneumoconiosis. There is a need to increase awareness that the presence of typical pneumoconiosis findings on radiological imaging obtained simultaneously can exclude other diagnoses and, thus, make a definitive diagnosis of pneumoconiosis.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Silica binding and toxicity in alveolar macrophages. Free Radic Biol Med. 2008;44:1246-58.
- [CrossRef] [PubMed] [Google Scholar]
- Silica-related diseases in the modern world. Allergy. 2020;75:2805-17.
- [CrossRef] [PubMed] [Google Scholar]
- Silicosis: An update and guide for clinicians. Clin Chest Med. 2020;41:709-22.
- [CrossRef] [PubMed] [Google Scholar]
- New insights into pathomechanisms and treatment possibilities for lung silicosis. Int J Mol Sci. 2021;22:4162.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of occupational lung disease. Radiol Clin North Am. 2016;54:1077-96.
- [CrossRef] [PubMed] [Google Scholar]
- Update on respiratory disease from coal mine and silica dust. Clin Chest Med. 2002;23:811-26.
- [CrossRef] [PubMed] [Google Scholar]
- Female workers' silicosis diagnosis delayed due to gender bias. Occup Med (Lond). 2019;69:219-22.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis of patients with silicosis due to denim sandblasting. Chest. 2012;141:831.
- [CrossRef] [PubMed] [Google Scholar]
- Screening and surveillance of workers exposed to mineral dusts Geneva: World Health Organization; 1996.
- [Google Scholar]
- Localized pneumoconiosis manifested by solitary pulmonary nodule mimicking lung cancer: One case report. Korean J Thorac Cardiovasc Surg. 2002;35:611-5.
- [Google Scholar]
- Progressive massive fibrosis mimicking lung cancer: Two case reports with potentially useful CT features for differential diagnosis. J Korean Soc Radiol. 2022;83:1175-81.
- [CrossRef] [PubMed] [Google Scholar]







