Translate this page into:
“Miliary lung parenchymal opacities” as presenting feature of metastatic papillary type of thyroid malignancy: It’s not tuberculosis always!

-
Received: ,
Accepted: ,
How to cite this article: Patil S, Mirza M, Gondhali G. “Miliary lung parenchymal opacities” as presenting feature of metastatic papillary type of thyroid malignancy: It’s not tuberculosis always! Glob J Health Sci Res. 2024;2:45-9. doi: 10.25259/GJHSR_52_2023
Abstract
Pulmonary tuberculosis (TB) is the most common cause of mortality and morbidity in South East Asia due to infective causes and tops the list of all infectious etiologies in India. Radiological presentations in pulmonary TB are diverse with the most common in them, which are nodules, consolidation, cavitation, and lung parenchymal destruction with or without collapse and consolidation. In this case report, a 31-year-old female presented with constitutional symptoms with miliary opacities in chest X-ray without microbiological evidence for TB in smear microscopy or nucleic acid amplification tests. She was treated as a case of miliary TB with antituberculosis treatment (ATT) on two occasions in the past 2 years as an “X-ray-positive case” on the basis of symptoms and chest radiology findings. She was never shown any clinical and radiological response in the past 1½ years in spite of satisfactory ATT adherence and compliance. After retrospective analysis of this case at our center, we have documented worsening of radiological findings and chest high-resolution computed tomography conformed miliary nodules and not typical miliary mottling favoring TB. We have noted right thyroid enlargement with a nodule in contrast tomography of neck. Fine-needle aspiration cytology confirmed as papillary carcinoma of the thyroid. We have confirmed this case as miliary metastasis due to primary thyroid malignancy. Miliary metastasis should be considered in cases with atypical radiological and clinical presentations with negative microbiological workup. No empirical ATT should be offered in the era of highly sensitive nucleic acid amplification tests and the term “X-ray-positive with negative microbiological tests” should be phased out.
Keywords
Miliary opacities
Miliary tuberculosis
Antituberculosis treatment
Miliary metastasis
Thyroid carcinoma
Acid-fast bacilli
Gene Xpert MTB/Rif
INTRODUCTION
Tuberculosis (TB) continues to be a major threat to global health. Miliary TB is a potentially fatal form of the disseminated disease due to the hematogenous spread of tubercle bacilli to the lungs, and other organs. It results in the formation of millet seed-sized (1–2 mm) tuberculous foci. The term miliary TB was first coined by John Jacobus Manget in 1700 while describing a pathological specimen having tiny tubercles similar to millet seeds in appearance. It originated from Latin word miliarius, related to millet seed. Disseminated TB is defined as simultaneous involvement of at least two non-contiguous organ sites of the body, or infection of the blood, bone marrow, or liver. Miliary mottling on a chest radiograph is the classical hallmark which supports the diagnosis of miliary TB. Miliary TB is classified as both pulmonary and extrapulmonary TB.[1] Pulmonary TB can have diverse presentations ranging from cavitation, consolidation, tumorous lesions, coin lesions, lower lung filed TB, and endobronchial and miliary nodules.[2-12] Similarly, non-tuberculous pathologies can present with abnormalities such as consolidations, nodules, and cavitations mimicking TB.[2-14] Bronchoscopy is a very crucial interventional pulmonology technique in evaluating these cases.[2-14] High-risk factors for TB would be advanced age, malnutrition, pregnancy, steroids exposure, diabetes mellitus, and immunosuppression.[2-12]
CASE REPORT
A 31-year-old female, farmer by occupation without any addiction history or any comorbidity was referred by a family physician to our center with a history of cough and shortness of breath of one and half year duration for further workup and treatment. Retrospectively, we have evaluated her chest X-ray examination at the start of antituberculosis treatment (ATT) and documented radiological abnormality. Chest X-ray was showing bilateral, multiple, randomly placed, tiny, and opacities in all lung zones predominantly dense in the middle and lower zones as compared to the upper zone [Figure 1a]. These opacities are diagnosed as miliary opacities and due to constitutional symptoms of cough and shortness of breath; these are labeled as miliary tuberculosis. She was treated as an X-ray-positive case as narrated by relatives. She was treated as per national TB elimination program at the primary health-care center for 6 months.
General physical examination documented as restless, thin-built young female with normal body temperature, and dry mucosa. Cyanosis and clubbing were noted. Her heart rate was 118/min, respiratory rate was 30 breaths/min, and blood pressure was 110/60 mmHg. His oxygen saturation was 81% at room air during resting and 89–96% during a routine walk with oxygen supplementation at the rate of 2 L/min by nasal cannula. Respiratory system examination revealed bilateral breath sounds normal and adventitious sounds as bilateral fine crepitation heard bilateral lung fields in the lower axillary and interscapular area. The swelling was confirmed as diffuse thyroid enlargement with a nodule on palpation which was moving with swallowing and confirmed clinically as thyroid nodule.
We have repeated chest X-ray in indoor unit which has documented worsening of miliary opacities [Figure 1b]. Miliary opacities are denser and more conglomerated in the lower zones to form ill-defined masses. Nodules are more in number, larger in size, and craniocaudal discordance is noted [Figure 1b]. We have evaluated with high-resolution computed tomography (HRCT) thorax and computed tomography (CT) neck with contrast study for lung parenchymal and thyroid pathology analysis.
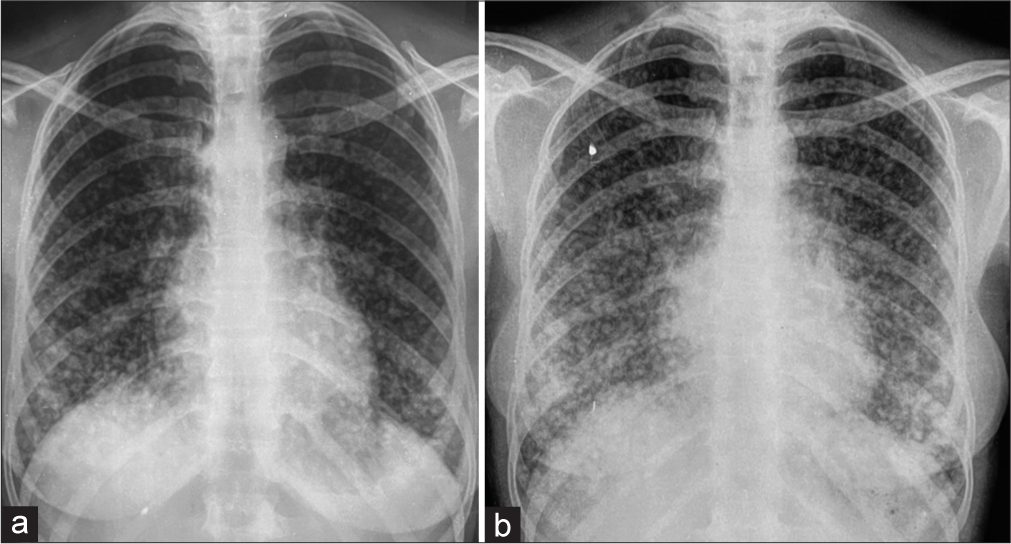
- (a and b) Chest X-ray PA showing consolidation in the right middle and lower zone.
High-resolution computed tomography thorax
Bilateral lung parenchymal nodular opacities, denser in the middle lobe, lingual, and both lower lobes as compared to the upper lobes [Figures 2 and 3]
Characteristically, these nodules are of variable size ranging from 3 mm to 8 mm, randomly distributed, bizarre shape, showing contrast uptake, and with interstitial enhancement favoring lymphohematogenous dissemination [Figures 2 and 3]
Multiple opacities are larger in size to label miliary mottling and showing craniocaudal discordance with conglomeration with contrast enhancement to favor non-tuberculous pathology [Figures 2 and 3]
Nodular opacities with an irregular shape, accompanied by conglomeration with parenchymal distortion in bilateral lower lobes without pleural or pericardial involvement [Figures 2 and 3].
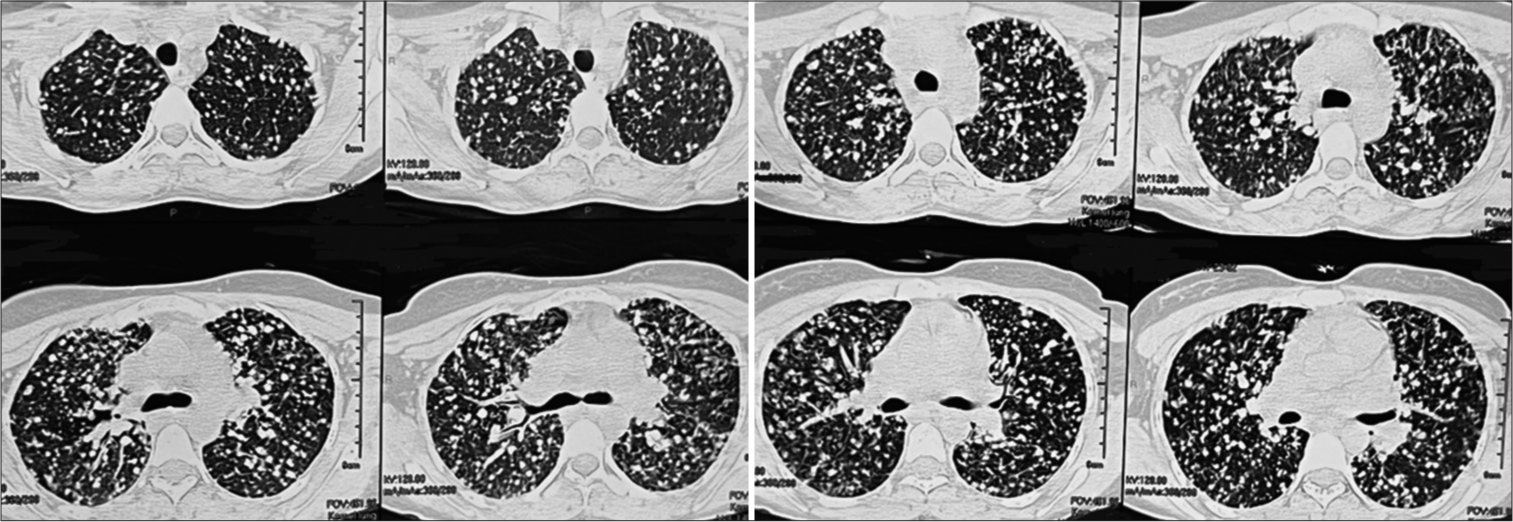
- High-resolution computed tomography thorax showing multiple, bilateral nodular opacities with craniocaudal discordance and conglomeration.
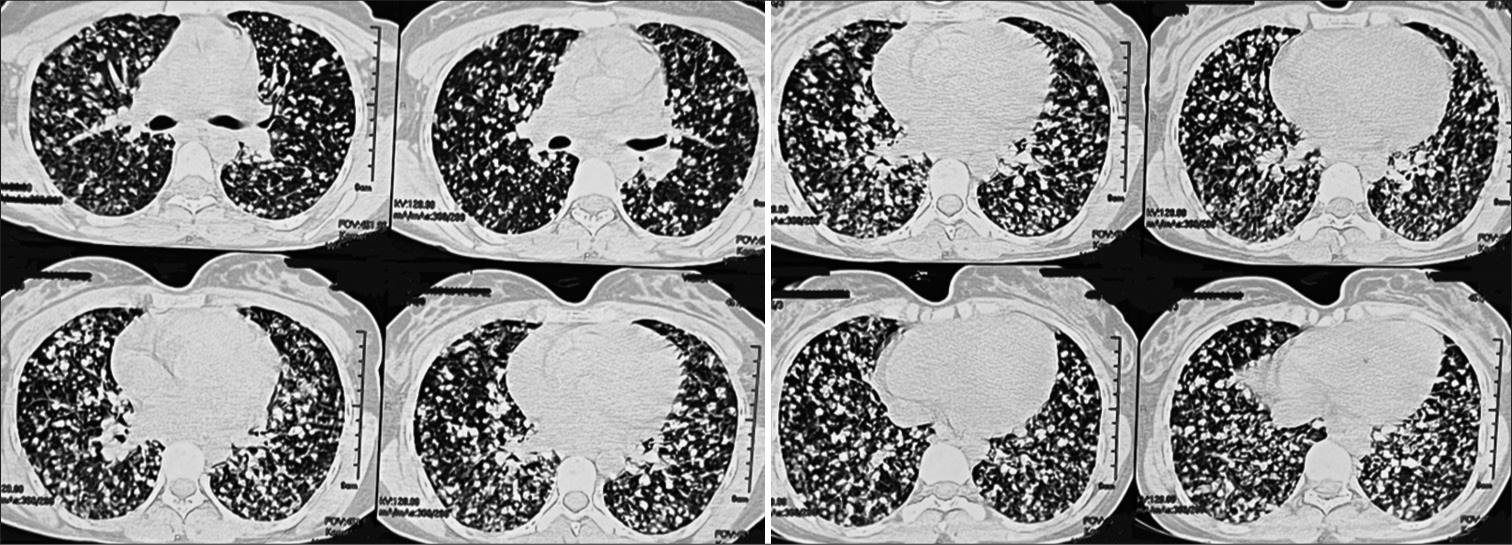
- High-resolution computed tomography thorax showing miliary nodule with conglomeration and parenchymal distortion in bilateral lower lobes with interstitial involvement.
CT neck
Bulky right lobe of the thyroid with hypodense thyroid nodule of size 2 cm × 1.7 cm noted in the right lobe with calcification and mild heterogeneous enhancement on contrast study mostly favors malignant pathology [Figure 4]
Multiple enlarged lymph nodes are seen at the bilateral jugular, submandibular, and right paratracheal region largest of size 23 mm × 17 mm at the right middle jugular region [Figure 4a-b].
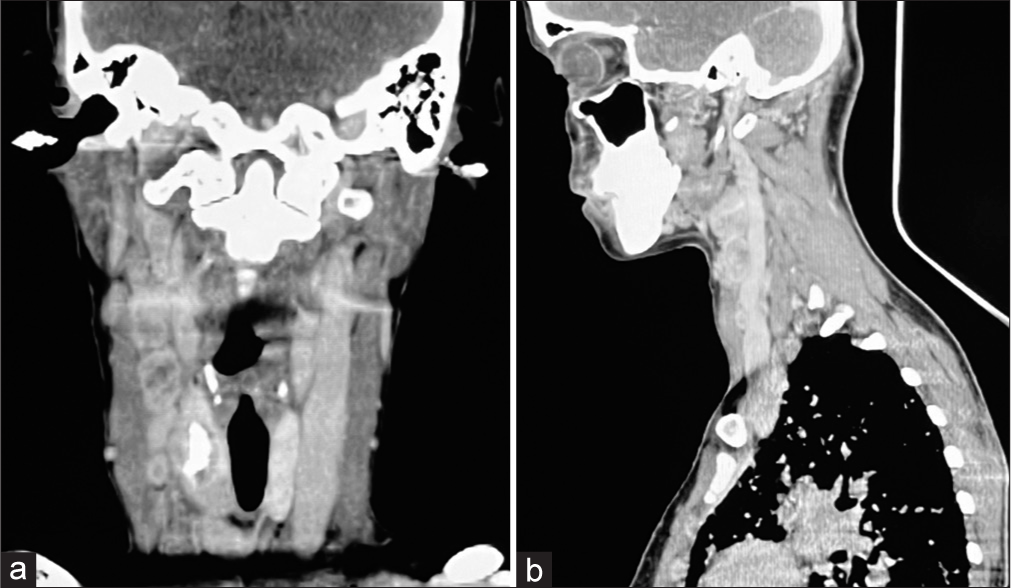
- (a and b) Computed tomography neck showing bulky right lobe of thyroid with hypodense thyroid nodule in the right lobe with calcification.
Percutaneous thyroid cytology smears show sheets and papillae like structures of follicular cells with well-defined anatomical border. The cells show powdery chromatin, nuclear grooves, intranuclear pseudo inclusions, and nuclear overlapping. Cytology analysis confirmed papillary type of thyroid carcinoma with Bethesda category VI.
We have referred this case to the tumor board of our institute after clinical parameter stability and general health improvement during hospitalization. In the tumor board panel, a multidisciplinary team of surgical oncologist, radiation oncologist, and medical oncologist decided on surgical removal of the thyroid with radioactive iodine therapy after surgery.
DISCUSSION
Miliary lung disease is characterized by the development of numerous small “millet seed” nodular lesions throughout the lungs, a pattern which indicates hematogenous or lymphatic spread. In such cases, accurate localization of pathologic change occurring within the lobule could be helpful in the differential diagnosis of certain pulmonary parenchymal diseases investigated by means of HRCT.
Miliary opacities due to tuberculosis and miliary metastasis: how to differentiate?
Size of nodules: Size <1.5 mm was more common in TB than malignancy. Nodule size of more than 3 mm was more frequently reported in miliary metastasis than TB. Nodule size between 1.5 mm and 3.0 mm is documented in miliary metastasis and TB in equal frequency[13]
Diversity in size of nodules: Variation in size of nodules is more frequently reported in miliary metastasis than miliary TB
Well-defined margins of nodules: Well-defined margins are commonly documented in TB and miliary metastasis. Ill-defined margins are a feature of metastasis than TB
Distributions as lower zone predominance or even distribution: Predominant lower zone is a typical feature of metastatic (70% cases) than miliary TB (30%). Even distribution of nodules is seen in miliary TB, that is, involvement of all zones equally. Even distribution is not common in miliary metastasis[14]
Coalescence or conglomeration: Common in miliary TB and miliary metastasis
Interstitial involvement is typically described as interlobular septal thickening or peribronchovascular thickening: Interstitial involvement is common in miliary metastasis and infrequently reported in TB
Ground-glass opacity: Common in TB and metastasis
Pleural effusion: Common in TB and metastasis
Lymph node enlargement: Common in TB and metastasis.
Papillary thyroid carcinoma (PTC) is the most frequent type with a ratio of 80%. PTC commonly metastasizes to regional lymph nodes. However, distant metastasis may rarely occur and accounts for 5% of the patients. The lungs and the bones are the most common sites for distant metastasis. Major risk factors for PTC include radiation exposure, insufficient or excess dietary iodine, Cowden’s disease, Gardner’s syndrome, and dyshormonogenetic goiter.[15]
CONCLUSION
In the present case report, we have documented miliary lung parenchymal opacities empirically treated as a case of tuberculosis without microbiological evidence. She was never evaluated for anything other than tuberculosis in spite of persistent radiological opacities and symptoms of neck swelling and altered voice. General examination revealed a thyroid mass in the right lobe and histopathology confirmed papillary carcinoma of the thyroid. We have confirmed papillary carcinoma of the thyroid presented with metastatic lung disease. Negative microbiological workup and nonresponding radiological disease to medical treatment was the real clue to think of a malignant cause for miliary lung metastasis.
Learning points
Constitutional symptoms with miliary opacities are more frequently reported in pulmonary TB. Miliary opacities are also observed in infectious, inflammatory, neoplastic, and interstitial lung diseases.
Conventional chest radiograph is a less sensitive technique to differentiate etiological factors for miliary TB as fine details of miliary opacities could not be possible and usually underestimated other causes for the same.
Although microbiological workup is indicated and must for diagnosis of TB, it is usually negative due to less or negligible expectoration in miliary TB. Induced sputum examination is superior to conventional sputum examination in miliary TB but less sensitive to bronchoscopy-guided samplings.
Empirical ATT with case definition as “X-ray-positive” without microbiological evidence and atypical radiological opacities and constitutional symptoms is always dangerous and should be phased out.
We recommend that etiological factors for miliary opacities should be actively sought, which will have an impact on the final outcome. Miliary TB is a common cause in India, and malignancy is not uncommon. Fine-needle aspiration is reliable, sensitive, and bedside test to diagnose thyroid neoplasms. Thus, we quote the slogan for miliary opacities as “It is not TB always for miliary opacities!”
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Miliary tuberculosis: New insights into an old disease. Lancet Infect Dis. 2005;5:415-30.
- [CrossRef] [PubMed] [Google Scholar]
- Cavitary lung disease: Not always due to tuberculosis! primary lung cancer with smear positive pulmonary tuberculosis-a case report. Am J Med Case Rep. 2014;2:164-6.
- [Google Scholar]
- Tuberculosis with diabetes mellitus: Clinical-radiological overlap and delayed sputum conversion needs cautious evaluation-prospective cohort study in tertiary care hospital, India. J Pulm Respir Med. 2014;4:175.
- [CrossRef] [Google Scholar]
- Tennis Racket cavity' on chest radiograph: Strong predictor of active pulmonary tuberculosis!-a case report. Am J Med Case Rep. 2014;2:167-9.
- [Google Scholar]
- Endobronchial tuberculosis presenting as a post-obstructive pneumonia, para-hilar mass lesion in chest radiograph and 'tumorous' Endobronchial lesion during bronchoscopy: A case report. Am J Infect Dis Microbiol. 2015;3:147-51.
- [Google Scholar]
- Coin lesion" in chest radiograph presenting as round pneumonia with eccentric cavitation in HRCT thorax: Tuberculosis or malignancy-a real puzzle! South Asian Res J Med Sci. 2023;5:33-40.
- [CrossRef] [Google Scholar]
- Stepladder lung cavities” with “starry sky pattern “in HRCT thorax with constitutional symptoms: A strong predictor of active pulmonary tuberculosis. SAR J Med. 2023;4:32-42.
- [CrossRef] [Google Scholar]
- Bronchial wash gene Xpert MTB/RIF in lower lung field tuberculosis: Sensitive, superior, and rapid in comparison with conventional diagnostic techniques. J Transl Intern Med. 2017;5:174-85.
- [CrossRef] [PubMed] [Google Scholar]
- Short course of high dose steroids used for non-pulmonary indication like anaphylaxis caused flare up of tuberculosis and presenting as acute pulmonary tuberculosis with pleural effusion: A case report. Eur J Gen Med. 2018;15:37-42.
- [CrossRef] [Google Scholar]
- Tuberculous lymphadenitis of hilar lymph nodes as a cause of right middle lobe syndrome: A case report. Respir Case Rep. 2018;7:90-6.
- [CrossRef] [Google Scholar]
- Fleeting pulmonary infiltrates in allergic bronchopulmonary aspergillosis" Misdiagnosed as tuberculosis. Int J Mycobacteriol. 2018;7:186-90.
- [CrossRef] [PubMed] [Google Scholar]
- Short course of high-dose steroids for anaphylaxis caused flare up of tuberculosis: A case report. J Transl Int Med. 2019;7:39-42.
- [CrossRef] [PubMed] [Google Scholar]
- CT of pulmonary metastases with pathological correlation. Semin Ultrasound CT MR. 1995;16:379-94.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of high-resolution CT findings between miliary metastases and miliary tuberculosis. J Korean Radiol Soc. 2003;48:147-52.
- [CrossRef] [Google Scholar]
- Papillary thyroid carcinoma with lung metastasis arising from dyshormonogenetic goiter: A case report. Case Rep Med. 2013;2013:813167.
- [CrossRef] [PubMed] [Google Scholar]







