Translate this page into:
Leber’s idiopathic stellate neuroretinitis - A clinical case

*Corresponding author: Vinitha Angalan, Department of Ophthalmology, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India. vinitha5126@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Angalan V, Renuga Devi K, Nallamuthu P. Leber’s idiopathic stellate neuroretinitis - A clinical case. Glob J Health Sci Res. doi: 10.25259/GJHSR_28_2024
Abstract
Neuroretinitis is a type of optic neuropathy characterized by an acute unilateral visual loss with optic disc swelling and macular star. A 26-year-old male presented with sudden blurring of vision in the right eye for 15 days. There were no other constitutional symptoms. On examination, visual acuity and color vision were impaired in the right eye. Visual-evoked potential showed a lower amplitude with increased latency on the right side. Perimetry showed centrocaecal scotoma. The right eye fundus showed a distinct neuroretinitis pattern Despite extensive investigation, no specific cause was identified, hence diagnosed as Leber’s idiopathic stellate neuroretinitis. The patient was started on oral prednisolone. Follow-up showed significant improvement.
Keywords
Idiopathic
Neuroretinitis
Cat scratch disease
Macular exudate
INTRODUCTION
Neuroretinitis is a sudden loss of vision in one eye due to swelling of the optic nerve head, often accompanied by star-shaped clusters of hard exudates near the retina’s center.[1] First described in 1916 by Theodore Leber, the condition, known as Leber’s Idiopathic Stellate Neuroretinitis (LISN), typically presents with unilateral symptoms, resolves spontaneously, and its exact cause remains uncertain. While usually of unknown origin, infectious diseases such as syphilis, Lyme disease, cat scratch disease, toxoplasmosis, and viral infections should be considered as potential triggers.[2,3]
CASE REPORT
A 26-year-old male visited outpatient department with a sudden onset of vision blurriness in his right eye lasting for 15 days. There were no other constitutional symptoms or contact with a pet animal. During examination, his right eye had an ill-sustained pupil and a best-corrected visual acuity of 6/12, which did not improve with a pinhole. His left eye had a visual acuity of 6/6. The anterior segment of both eyes appears normal. However, color vision was affected in the right eye. Visual field testing showed a centrocaecal scotoma in the right eye [Figures 1 and 2]. Fundus examination of the right eye revealed an optic nerve head with blurred edges, hyperemia, and star-shaped hard exudate deposited around the macula. Vessels originating from the optic nerve head were obscured, and veins appeared dilated and tortuous [Figures 3-5].
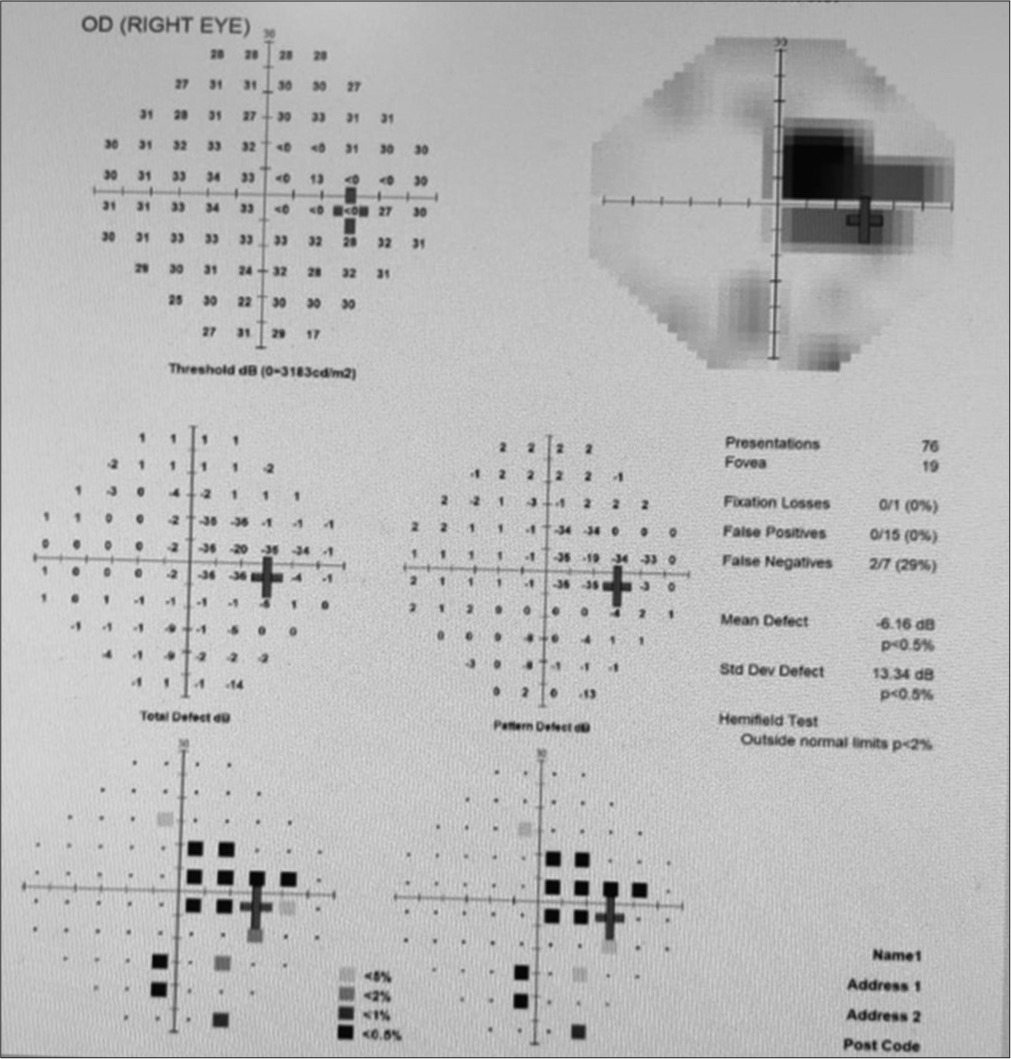
- Perimetery of the right eye, on the day of presentation showing centrocaecal scotoma.
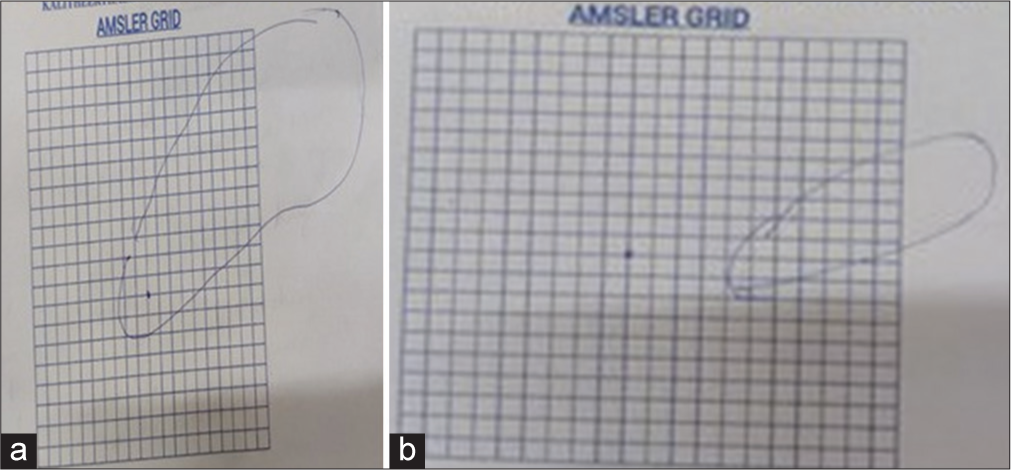
- (a) Amsler grid, on the day of presentation (marked by patient). (b) Amsler grid, on follow-up.
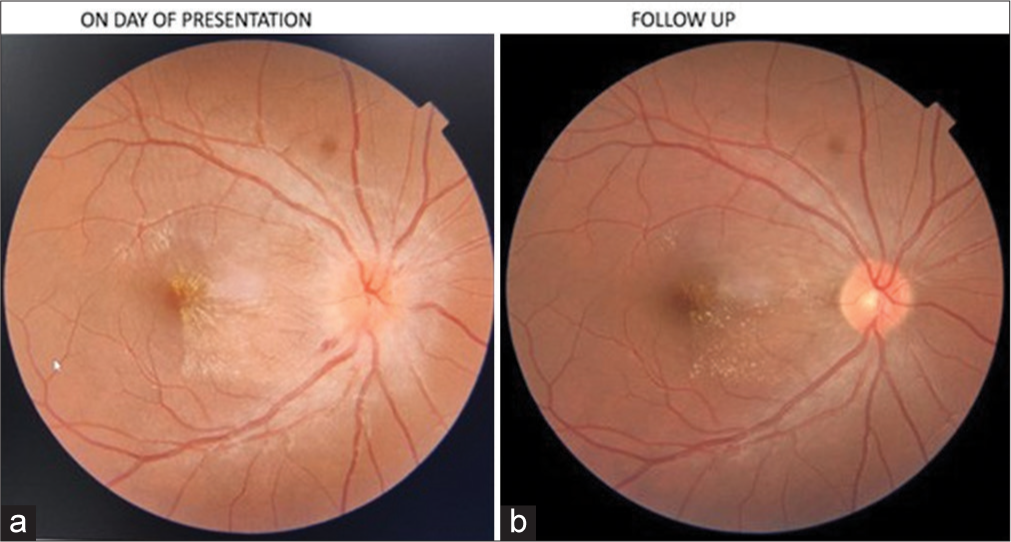
- (a) Optical coherence tomography (OCT) fundus of the right eye, on the day of presentation. (b) OCT fundus of right eye, on follow-up.
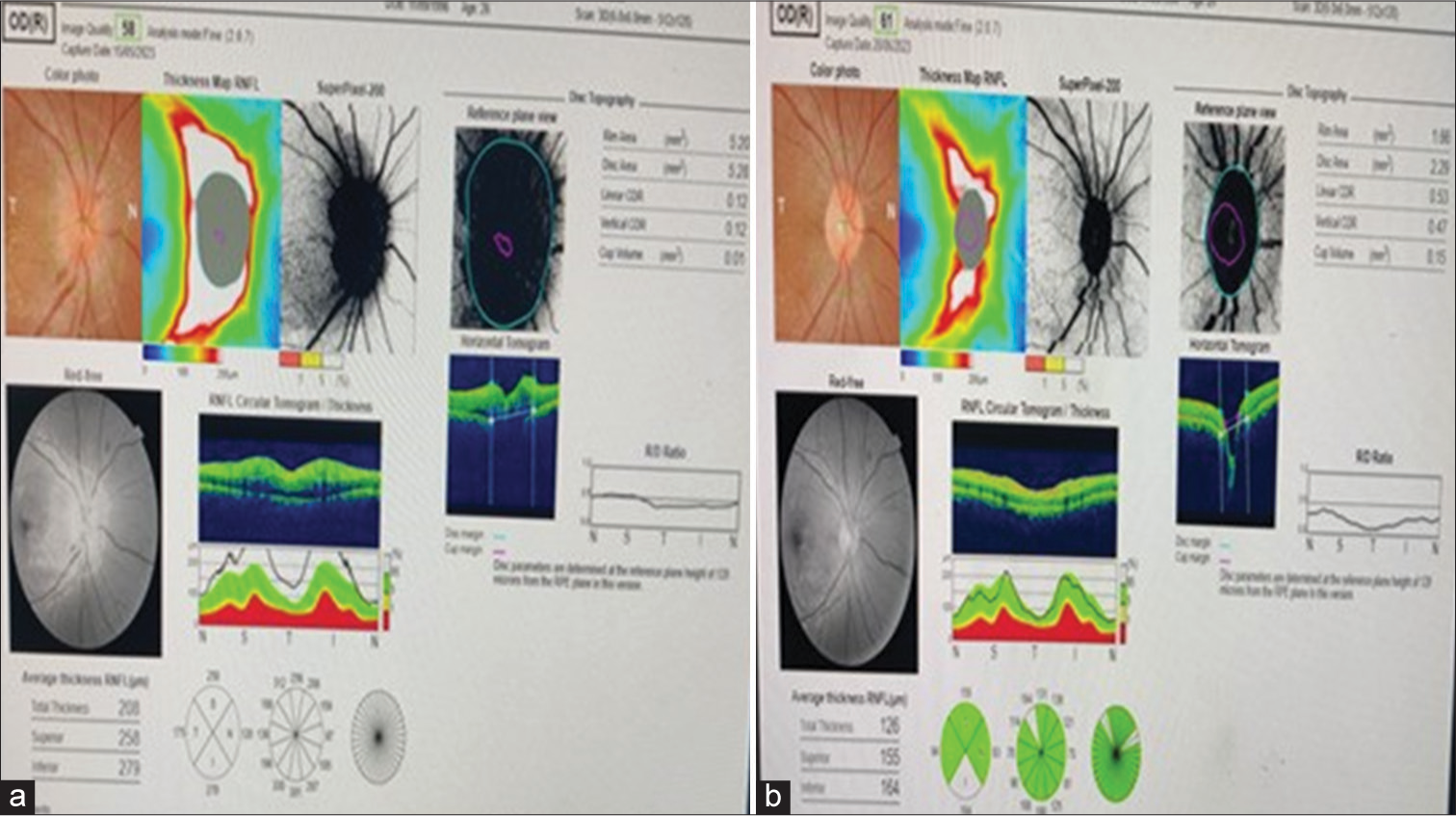
- (a) Optical coherence tomography (OCT) disc of the right eye on the day of presentation. (b) OCT disc of the right eye on follow-up.
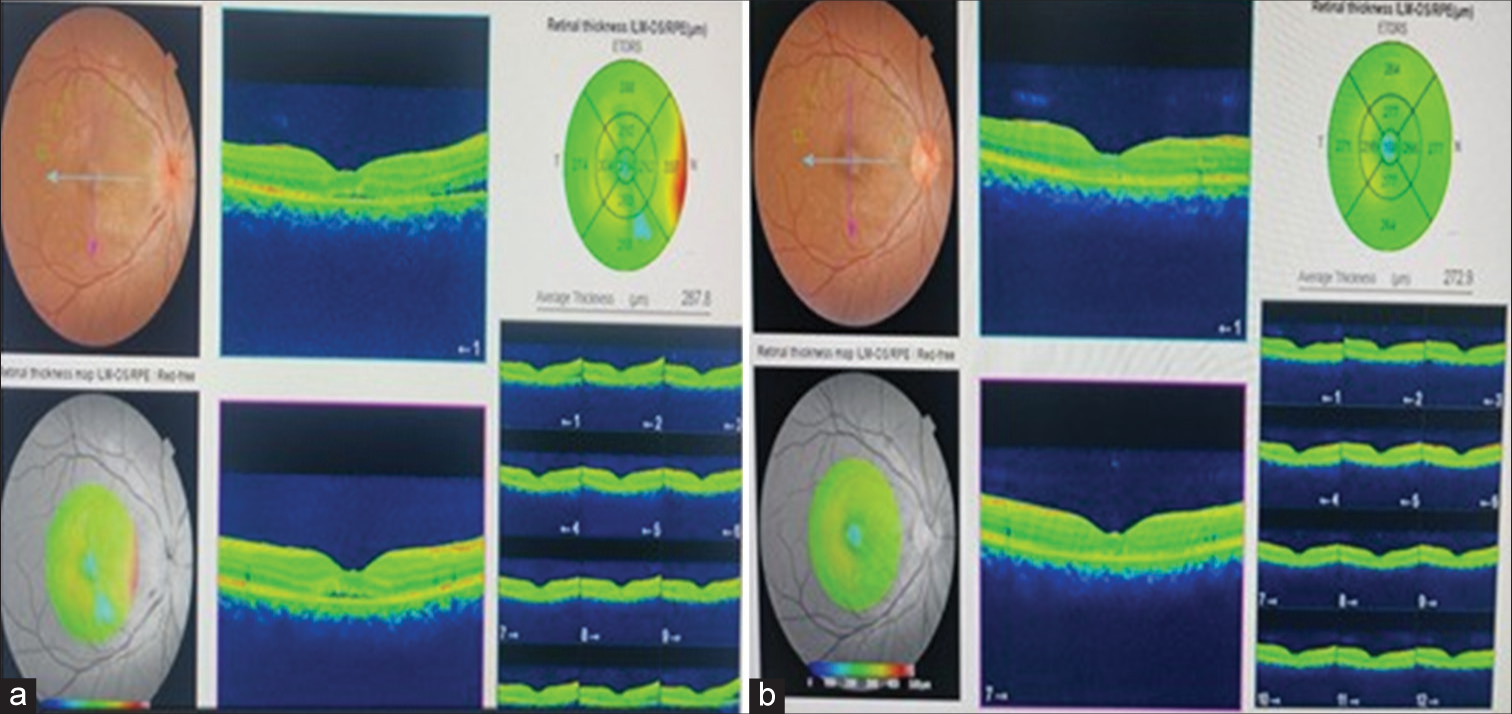
- (a) Optical coherence tomography (OCT) macula of the right eye on the day of presentation. (b) OCT macula of the right eye on follow-up.
Visual-evoked potential showed a lower amplitude on both sides with an increased latency of 107 ms on the right side and normal electroretinogram results. Fluorescein angiography revealed widespread leaking from the optic nerve head and macula. Ultrasound imaging of the right eye indicated optic nerve sheath widening and slight elevation of the optic nerve head by 1 mm. The other eye was unremarkable. Other eye examinations were normal, including cranial nerves and neurological assessments. Investigations were carried out to find the secondary causes as per standard protocols. Imaging of the brain and optic nerve head showed no abnormalities. After a thorough examination, no specific cause was found, leading to a diagnosis of LISN. The patient was prescribed oral prednisolone starting at 40 mg daily for 15 days, with a gradual tapering off. Follow-up assessments showed an improvement in vision to 6/9 after 2 weeks, along with a reduction in the size of the centrocaecal scotoma and macular edema. The optic nerve head in the right eye appeared healthier, with a cup-to-disc ratio of 0.3. While some residual macular exudate persisted, the patient did not experience any neurological symptoms throughout the follow-up period and remained asymptomatic.
DISCUSSION
Neuroretinitis is defined as inflammation of the anterior optic nerve head and peripapillary retina.[4] This inflammation leads to excessive leakage from the blood vessels around the optic disc, causing fluid accumulation around the optic nerve head. Approximately 10 days later, hard exudate deposits form in a distinctive star-shaped pattern, typically tracking toward the macula.[5] LISN is a specific type of this disorder, characterized by swelling of the optic nerve head, accumulation of hard exudate around the optic disc and macula, and often the presence of cells in the vitreous humor. Neuroretinitis often lacks a clear cause, but infectious factors such as syphilis, Lyme disease, cat scratch disease, toxoplasmosis, and viral infections should be considered. The exact cause of neuroretinitis remains unclear, though it is believed to result from either an infectious or immune-mediated process triggered by various agents.[6] While viral syndromes are commonly associated with neuroretinitis, viral cultures from eye fluid or cerebrospinal fluid are rarely positive, and serological evidence of viral infection is usually absent. Possible viral agents include herpes simplex, hepatitis B, mumps, and herpes viruses linked to acute retinal necrosis syndrome. Other infections implicated in neuroretinitis include cat scratch disease, syphilis, Lyme disease, leptospirosis, toxoplasmosis, toxocariasis, and histoplasmosis.
According to Dreyer et al., when the cause of the disease cannot be pinpointed, it is labeled as Leber’s idiopathic stellate retinopathy.[7] Almost 50% of cases have no identifiable cause and are labeled as idiopathic neuroretinitis.[8] Some evidence even indicates that Leber’s neuroretinitis is nothing but a manifestation of Cat scratch disease, but the extent of association remains to be determined.[9] This diagnosis is reached after excluding other known causes of neuroretinitis. It typically affects young, healthy individuals and manifests as sudden vision loss in one eye. While systemic steroid treatments have been tried, there is no solid evidence that they significantly impact the speed of recovery or the outcome. In general, the prognosis is favorable, with spontaneous improvement usually occurring within 6–12 weeks.[10] However, the star-shaped pattern around the macula might persist beyond this timeframe.
In the mentioned case, despite thorough evaluation, no specific cause was identified, leading to a diagnosis of LISN. While the condition typically resolves on its own, patients are often given steroid treatment during the acute phase. In cases with no identifiable cause, the overall prognosis for visual recovery is generally positive, as observed in this instance.
CONCLUSION
When encountering optic disc swelling combined with star-shaped macular exudate, it is crucial to exclude all treatable conditions before settling on a diagnosis of LISN. While its fundoscopic appearance aids in distinguishing it from typical optic neuropathies, neuroretinitis can imitate various disorders, complicating diagnosis. In cases lacking a clear cause, vision typically improves over weeks to months. However, the efficacy of steroid therapy in such cases remains uncertain.
Acknowledgment
I would like to acknowledge the department of neurology, for their expertise and assistance throughout all aspects of our study.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Leber's idiopathic stellate neuroretinitis: A clinical case. Ann Med Surg. 2022;76:103491.
- [CrossRef] [Google Scholar]
- Neuroretinitis, a great mimicker. Ann Indian Acad Neurol. 2008;11:109-13.
- [CrossRef] [Google Scholar]
- Recurrent idiopathic neuroretinitis: Natural history and effect of treatment. Clin Exp Ophthalmol. 2010;38:591-6.
- [CrossRef] [Google Scholar]
- Leber's idiopathic stellate neuroretinitis. Arch Ophthalmol. 1984;102:1140-5.
- [CrossRef] [Google Scholar]
- Treatment strategies for neuroretinitis: Current options and emerging therapies. Curr Treat Options Neurol. 2019;21:36.
- [CrossRef] [Google Scholar]
- Leber’s idiopathic stellate neuroretinitis. Apropos of 9 cases. J Fr Ophtalmol. 1994;17:116-23.
- [Google Scholar]







