Translate this page into:
Exploring Bangladeshi physicians’ attitudes toward mobile health apps

*Corresponding author: Samia Amin, Department of Public Health, Macquarie University, Sydney, New South Wales, Australia. drsamia27@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Amin S, Saha P, Sazal R. Exploring Bangladeshi physicians’ attitudes toward mobile health apps. Glob J Health Sci Res. 2025;3:33-6. doi: 10.25259/GJHSR_26_2024
Abstract
Objectives:
Mobile Health (mHealth) apps have emerged as transformative tools with the potential to revolutionize health-care delivery, particularly in resource-constrained settings like Bangladesh. This cross-sectional study aimed to explore the trends of use of mHealth apps among Bangladeshi physicians and assess their attitudes toward integrating these apps into the health-care system.
Material and Methods:
Data were collected from 120 physicians using structured questionnaires, addressing awareness, usage patterns, barriers, and future considerations related to mHealth apps. Descriptive statistical analyses were conducted to identify factors influencing mHealth app adoption and attitudes among Bangladeshi physicians.
Results:
The results indicated a relatively high level of engagement with mHealth apps among Bangladeshi physicians, with 63.3% reporting personal usage for health monitoring. However, variability in recommendation practices and integration into clinical workflows highlighted challenges in adoption. Barriers to adoption included lack of awareness, security concerns, and technological barriers. Despite these challenges, a significant proportion of physicians expressed willingness to consider adopting mHealth apps in the future.
Conclusion:
The findings of this study underscore the need for targeted interventions to address barriers to mHealth app adoption and promote their effective integration into Bangladesh’s health-care system. Recommendations include targeted educational initiatives, addressing infrastructure barriers, and fostering collaboration among stakeholders. By leveraging mHealth technology, Bangladesh can advance toward a more accessible, efficient, and patient-centered health-care delivery model.
Keywords
mHealth
Mobile health app
Physician
Bangladesh
INTRODUCTION
In recent years, the landscape of health-care delivery has been significantly transformed by the rapid advancement of mobile technology.[1] Mobile Health (mHealth) apps, accessible through smartphones and other portable devices, have emerged as potent tools with the potential to revolutionize health-care accessibility, delivery, and patient engagement.[1] These applications offer a diverse array of functionalities, ranging from health monitoring and data tracking to teleconsultation services and personalized health interventions.[2] In the context of Bangladesh, where health-care resources are often constrained and access to medical services can be challenging, the integration of mHealth apps holds particular promise for overcoming barriers to health-care delivery and improving health outcomes.
However, the successful implementation of mHealth apps into the Bangladeshi health-care system hinges on the attitudes and adoption practices of key stakeholders, notably physicians. As frontline health-care providers, physicians play a pivotal role in shaping the use and integration of technological innovations within clinical practice.[3] Understanding their perceptions, usage patterns, and attitudes toward mHealth apps is paramount for devising effective strategies to leverage these technologies optimally.[4] Moreover, given the diverse sociodemographic and health-care landscape of Bangladesh, a nuanced exploration of the trends and attitudes toward mHealth app utilization among Bangladeshi physicians is essential for tailoring interventions and policies to the unique needs and challenges of the local health-care ecosystem.[5] Therefore, this cross-sectional study aims to fill this crucial knowledge gap by exploring the trends of use of mHealth apps among Bangladeshi physicians and assessing their attitudes toward integrating these apps into the health-care system.
MATERIAL AND METHODS
This study employed a cross-sectional design, using a convenient sampling technique. The sampling frame comprised licensed physicians practicing in various health-care settings across Bangladesh. Data collection was conducted over 3 months, from January to March 2024.
Data were collected using structured questionnaires which were designed based on a thorough review of existing literature on mHealth app awareness, usage, and attitudes.[6-8] It underwent iterative refinement through expert consultation and pilot testing to ensure clarity, relevance, and validity. The finalized questionnaire consisted of sections addressing demographic characteristics (age, gender, and level of education) and attitudes toward mHealth app integration into the health-care system. The survey encompassed the following questions: (A) Awareness and familiarity: (i) How familiar are you with mHealth apps? (ii) What specific types of mHealth apps are you aware of? (B) Usage and adoption: (iii) Have you ever used any mHealth apps for your health monitoring? (iv) How often do you recommend the use of health apps to patients? (v) Have you personally adopted the use of mHealth apps in your medical practice? (vi) If yes, how frequently do you use mHealth apps for patient-related activities? (C) Barriers and future considerations: (vii) If no, what factors have prevented you from adopting mHealth apps in your practice? and (viii) How likely are you to consider adopting mHealth apps in your practice in the future?
The distribution of questionnaires was carried out through both physical and electronic channels, depending on participants’ preferences and logistical considerations. For physical distribution, trained research assistants visited health-care facilities and distributed the questionnaires to eligible physicians. For electronic distribution, participants were contacted through email or messaging platforms, and a secure link to the online questionnaire was provided. Clear instructions were provided to participants regarding questionnaire completion, ensuring consistency and data quality. Anonymity and confidentiality were assured throughout the data collection process to encourage honest responses.
Descriptive statistical analyses were performed to identify factors influencing mHealth app adoption and attitudes among Bangladeshi physicians. Statistical software packages SPSS was utilized for data analysis. Informed consent was obtained from all participants before their involvement in the study, emphasizing voluntary participation and the right to withdraw at any time without repercussion.
RESULTS
Demographic information
Out of the 120 respondents, the majority were between the ages of 30 and 40, reflecting a relatively young cohort of physicians engaging with the survey. Gender distribution indicated a slight male predominance, with 62.5% male and 37.5% female respondents. The highest level of education varied, with a significant proportion holding M.B.B.S degree followed by post-graduation qualifications (21.7%).
Awareness and familiarity
Approximately 60.9% of respondents reported being either somewhat familiar or very familiar with mHealth apps. The types of mHealth apps recognized by respondents included those for health record management, telemedicine/telehealth, medication reminders, appointment scheduling, and remote patient monitoring.
Usage and adoption
About 63.3% of respondents had used mHealth apps for personal health monitoring, while 35.8% had not. Regarding the recommendation of health apps to patients, responses varied, with a notable proportion reporting rarely or never recommending such apps [Figure 1]. While nearly half (48.3%) of the respondents had personally adopted the use of mHealth apps in their medical practice, the frequency of usage for patient-related activities varied among them.
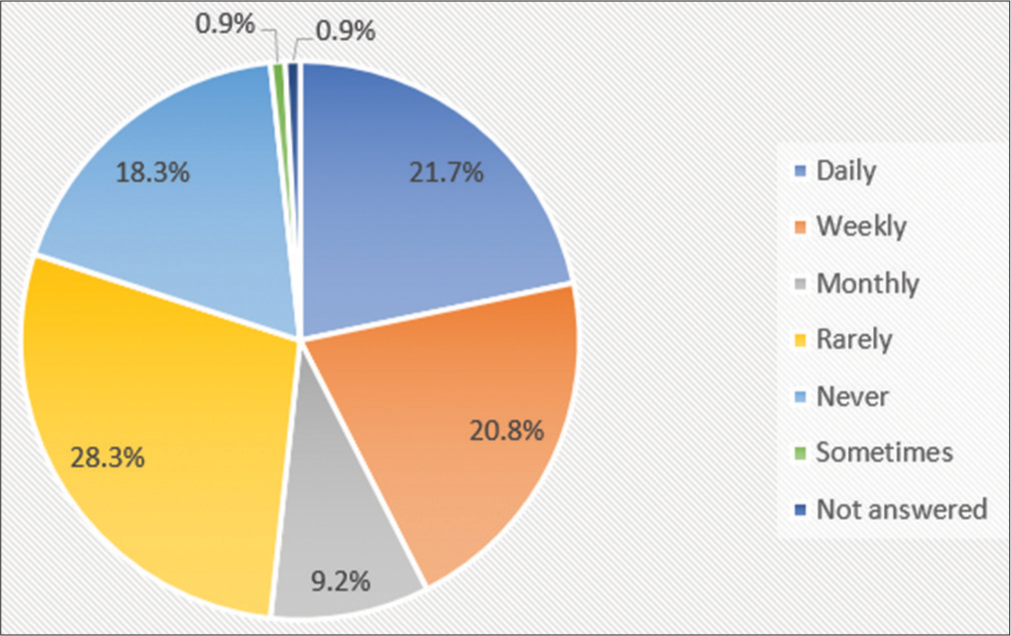
- Physician’s (n = 120) recommendation to patients on using health apps.
Barriers and challenges
Factors hindering the adoption of mHealth apps included lack of awareness, security concerns, technological barriers, time constraints, personal preferences, and lack of interest.
Future considerations and attitudes toward integration
Despite existing barriers, a significant proportion of respondents expressed a willingness to consider adopting mHealth apps in their practice in the future [Figure 2].
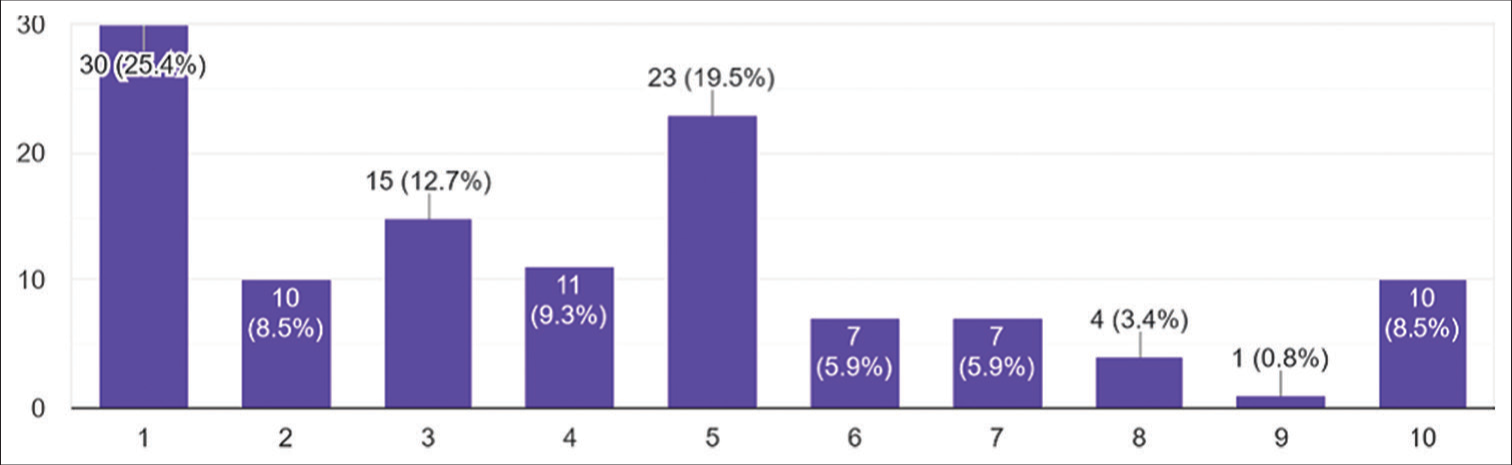
- Physician’s (n = 118) consideration adopting mobile health apps in the future.
DISCUSSION
The results of this study provide valuable insights into the usage patterns and attitudes toward mHealth apps among Bangladeshi physicians. The survey revealed that a significant proportion of respondents (63.3%) had utilized mHealth apps for personal health monitoring, indicating a relatively high level of engagement with digital health tools among physicians in Bangladesh. However, there was considerable variability in the frequency of recommending these apps to patients and integrating them into clinical practice. While some physicians embraced mHealth apps as integral components of patient care, others exhibited more cautious or reserved approaches. Barriers to adoption, including lack of awareness, security concerns, and technological barriers, were identified as key challenges hindering the widespread integration of mHealth apps into clinical workflows.
The findings of this study align with previous research documenting the growing recognition and adoption of mHealth apps among health-care professionals worldwide.[6-11] However, they also highlight unique challenges and opportunities specific to the Bangladeshi context. While studies conducted in other countries have reported similar barriers to adoption, such as concerns about data security and privacy, the prevalence and impact of these barriers may vary across different health-care settings and cultural contexts.[7,11] In addition, the variability in recommendation practices observed in this study underscores the importance of tailoring mHealth interventions to the specific needs and preferences of local health-care providers and patients.
Several limitations should be acknowledged when interpreting the findings of this study. First, the use of a convenience sampling method may limit the generalizability of the results to the broader population of Bangladeshi physicians. In addition, the cross-sectional design precludes the establishment of causal relationships between variables and may not capture temporal changes in usage patterns and attitudes toward mHealth apps over time. Furthermore, self-reported data may be subject to recall bias and social desirability bias, potentially influencing the accuracy of responses.
Despite these limitations, the study has several strengths. The inclusion of a diverse sample of physicians from different geographic regions and health-care sectors enhances the representativeness of the findings. Moreover, the use of structured questionnaires allowed for systematic data collection and analysis, facilitating the identification of key trends and patterns in mHealth app usage and attitudes. The findings contribute to the growing body of literature on digital health adoption in low-resource settings and provide valuable insights for policymakers, health-care providers, and technology developers seeking to promote the effective integration of mHealth apps into health-care delivery in Bangladesh.
Several recommendations can be made to promote the effective utilization of mHealth apps in Bangladesh’s health-care system. First, targeted educational initiatives are needed to raise awareness among health-care professionals about the benefits and functionalities of mHealth apps and address misconceptions and concerns. Second, efforts should be made to address infrastructure and technological barriers, such as limited internet connectivity and smartphone penetration, to ensure equitable access to mHealth solutions across diverse populations. In addition, collaboration between stakeholders, including government agencies, health-care providers, technology developers, and academic institutions, is essential for developing and implementing evidence-based mHealth interventions tailored to the specific needs and preferences of the Bangladeshi population. Finally, further research is needed to evaluate the effectiveness of mHealth interventions in improving health outcomes, patient satisfaction, and health-care efficiency in real-world settings, informing future policy and practice decisions. By addressing these recommendations, Bangladesh can harness the transformative potential of mHealth technology to advance toward a more accessible, efficient, and patient-centered health-care system.
CONCLUSION
This study provides a comprehensive overview of the attitudes and adoption practices of Bangladeshi physicians toward mHealth apps. The findings indicate that while a majority of physicians are familiar with and have used mHealth apps for personal health monitoring, there is significant variability in their integration into clinical practice and patient care. Key barriers such as lack of awareness, security concerns, and technological limitations hinder the widespread adoption of these digital tools. Despite these challenges, there is a notable willingness among physicians to consider incorporating mHealth apps in the future, highlighting an opportunity for targeted interventions to facilitate this process.
To harness the potential of mHealth technology in improving health-care delivery in Bangladesh, it is essential to address the identified barriers through educational initiatives, infrastructure improvements, and collaborative efforts among stakeholders. By doing so, mHealth apps can be effectively integrated into the health-care system, enhancing accessibility, efficiency, and patient-centered care. Further research is recommended to evaluate the long-term impacts of mHealth interventions on health outcomes and to develop tailored strategies that align with the unique needs of the Bangladeshi health-care ecosystem.
Ethical approval
Ethical approval was not required for this study as the data utilized was completely de-identified and anonymous, ensuring no risk of identifying individual participants.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Mobile devices and apps for health care professionals: Uses and benefits. P T. 2014;39:356-64.
- [Google Scholar]
- The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLoS Med. 2013;10:e1001363.
- [CrossRef] [Google Scholar]
- The use of medical health applications by primary care physicians in Israel: A cross-sectional study. BMC Health Serv Res. 2024;24:410.
- [CrossRef] [Google Scholar]
- The impact of mhealth interventions: Systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6:e23.
- [CrossRef] [Google Scholar]
- eHealth and mHealth initiatives in Bangladesh: A scoping study. BMC Health Serv Res. 2014;14:260.
- [CrossRef] [Google Scholar]
- Mobile health applications: Awareness, attitudes, and practices among medical students in Malaysia. BMC Med Educ. 2022;22:544.
- [CrossRef] [Google Scholar]
- Knowledge, attitude and practice toward the mHealth app Mawid: A cross-sectional study. Int Health. 2023;15:342-50.
- [CrossRef] [Google Scholar]
- Attitudes of general practitioners toward prescription of mobile health apps: Qualitative study. JMIR mHealth uHealth. 2021;9:e21795.
- [CrossRef] [Google Scholar]
- Physician attitudes towards-and adoption of-mobile health. Digit Health. 2020;6:2055207620907187.
- [CrossRef] [Google Scholar]
- Factors affecting physicians using mobile health applications: An empirical study. BMC Health Serv Res. 2022;22:24.
- [CrossRef] [Google Scholar]
- Willingness of French general practitioners to prescribe mhealth apps and devices: Quantitative study. JMIR Mhealth Uhealth. 2022;10:e28372.
- [CrossRef] [Google Scholar]







