Translate this page into:
Clinical audit on postpartum hemoglobin levels: A study on postpartum anemia

*Corresponding author: Kulkarni Sweta, Department of Biochemistry, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India. shwetakulkarni82@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: John J, Arsha AR, Balamurugan S, Athipozhi Thomas T, Sweta K, Kasilingam P, et al. Clinical audit on postpartum hemoglobin levels: A study on postpartum anemia. Glob J Health Sci Res. 2025;3:37-42. doi: 10.25259/GJHSR_24_2024
Abstract
Objectives:
The present study was carried out to assess the prevalence of anemia with reference to the Hb levels during postpartum period. The study also investigates the influence of age and mode of delivery on postpartum Hb levels.
Material and Methods:
It is a hospital-based retrospective descriptive study. The postpartum patients’ data were obtained from the medical records department of a tertiary care hospital. Data of the patients registered for routine blood investigation in the period of December 2023 to January 2024 were collected from the records. Based on patient’s hospital ID, other details including age, Hb level, and mode of delivery data were obtained. Statistical analysis was performed to check the effect of age and mode of delivery on postpartum Hb level by Pearson correlation using IBM Statistical Package for the Social Sciences Statistics version 24.0.
Results:
About 64.3% of the patients belonged to the age group of 20–30 years and remaining 35.7% within 30–40 years. The percentage of postpartum patients who underwent lower segment cesarean section (LSCS) and normal vaginal delivery (NVD) were 85.7% and 14.3%, respectively. However, cumulative percentage of NVD was higher (100%) than LSCS (85.7%). The postpartum Hb level ranged from 7.9 to 15.2 g/dL. About 54% of patients showed moderate anemia (8–10.9 g/dL), followed by 24% mild (11.9–11 g/dL) and 2% with severe anemic (<8 g/dL) condition.
Conclusion:
The study highlights the prevalence of PPA associated with both LSCS and NVD modes of delivery. Although the number of anemic patients was higher in LSCS (48) compared to NVD (8), the percentage remains the same at 80% each considering the total number of patients in each category. These observations point out the risk of high-volume blood loss associated with both modes of delivery and emphasize the need for adopting precautionary measures.
Keywords
Hemoglobin level
Lower segment caesarian section
Normal vaginal delivery
Postpartum anemia
INTRODUCTION
Hemoglobin (Hb) in red blood cells (RBCs) acts as a carrier to transport oxygen from the lungs to tissues and organs through blood. It is a protein that contains iron and its deficiency could lead to insufficient oxygen supply in the body. During pregnancy, the mother requires more iron to meet the increase in blood volume and to enhance the oxygen transport to the baby. The normal Hb level in women is 12–16 g/dL and anemia arises if Hb content falls below the prescribed level.[1]
Postpartum anemia (PPA) is a low Hb concentration of <11 g/dL at 24–48 h after childbirth and ought to be considered severe at Hb level <8 g/dL. In general, delivery of placenta is followed by postpartum period which lasts up to 42 days and is considered as the crucial period of mother and infant’s health and survival.[2] PPA is an escalating and severe form of maternal morbidity that affects up to 50–80% of women after child delivery. Worldwide, PPA remains a serious and enduring public health problem which could be preventable with awareness and implementation of adequate management strategies.[3] The most common causes of PPA are iron deficiency before birth or severe bleeding during birth and serious health issue in women in the reproductive age. Women with PPA experience health-related quality of life including increased risk post-partum hemorrhage, emotional instability, palpitations, depression, insufficient milk syndrome, and reduced cognitive function.[4-8] Preferred treatment choices for PPA patients are administration of intravenous (IV) iron, oral iron, and RBC transfusion (RBC-T). Without treatment, daily activities of PPA patients often met with difficulties after delivery. Therefore, when PPA is higher, it is highly advised to take up medical treatment and the most recommended options are IV-iron and RBC-T.[4]
In India, the prevalence of PPA is estimated at 65%, highlighting the fact that it is a major public health problem. Since it is one of the silent factors contributing to maternal morbidity, it is important to assess Hb levels in women at a community level during postpartum period. We hypothesize that age of PPA patients and mode of delivery could be influential in determining the Hb levels in PPA patients. Hence, this study was proposed to evaluate the Hb levels in postpartum periods and investigate the association of age and mode of delivery of postpartum mothers on their Hb concentrations.
MATERIAL AND METHODS
Study design
It is a hospital-based retrospective descriptive study conducted over 2-month period prospectively from December 1, 2023, to January 31, 2024, among postpartum women attending a tertiary care hospital.
Study setting and population
Postpartum patients between the age of 20 and 40 years who were undergone vaginal and cesarean delivery and are enrolled for the estimation of Hb level as of December 2023 till January 2024 were considered for the study. Background and clinical information related to postpartum patients were obtained from the medical records department (MRD) of the tertiary care hospital. The study and related data analysis were carried out in the Central Research Laboratory, SMVMCH.
Sample size
Based on the records from MRD, data from 70 postpartum patients registered in the prescribed time period were included in the study.
Data collection procedure
After obtaining consent from authority, hospital IDs of postpartum mothers enrolled for the estimation of Hb levels in the period of December 2023–January 2024 were collected from the laboratory registers. Further, based on the patient’s ID, details such as age, Hb level, and mode of delivery (lower segment cesarean section [LSCS] or normal vaginal delivery [NVD]) of each patient were obtained from MRD.
Statistical analysis
Data obtained from MRD are represented as range, mean with standard deviation or percentage as appropriate. Valid and cumulative percentages were calculated for those undergone LSCS and NVD. The impact of age and mode of delivery as the risk factors on Hb level was evaluated through linear regression by Pearson correlation analysis using IBM Statistical Package for the Social Sciences Statistics version 24.0 (IBM Co., Armonk, NY, USA). A comprehensive flow chart of the study is depicted in Figure 1.
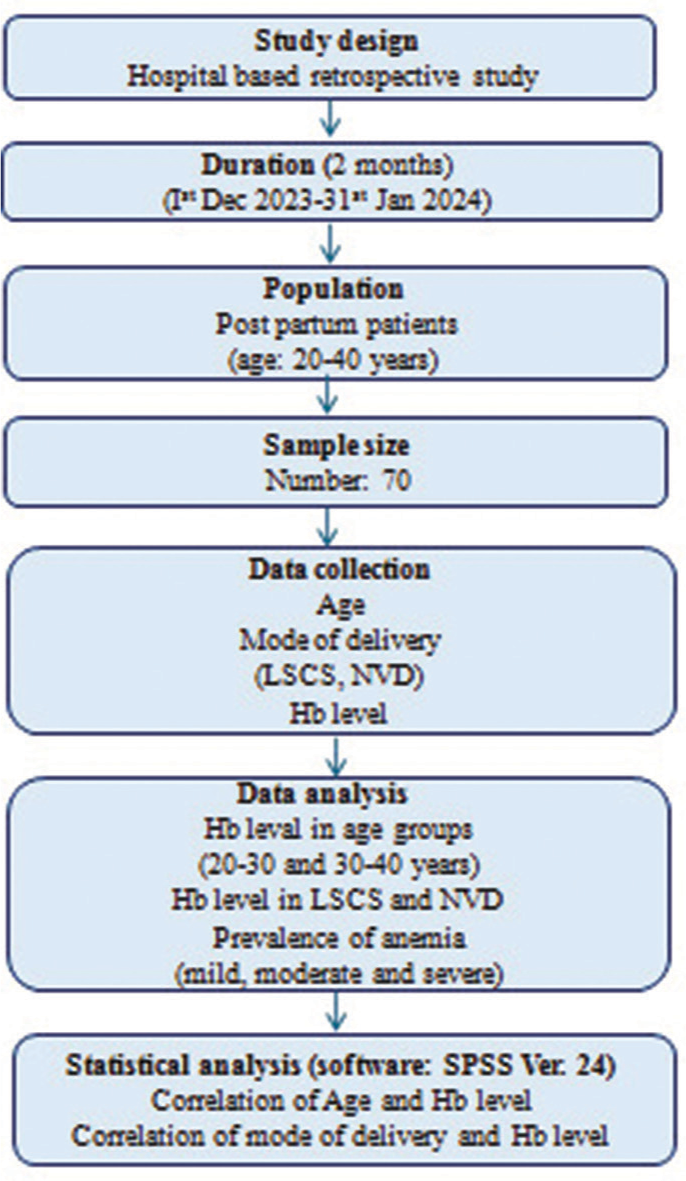
- Flow chart of the retrospective study on PPA. PPA: Postpartum anemia, Hb: Hemoglobin, LSCS: Lower segment cesarean section, NVD: Normal vaginal delivery.
RESULTS
Age distribution of postpartum mothers
Data from 70 women in the postpartum phase were considered for the study. Age of the mothers varied from 20 to 39 years with a mean value of 25 and was divided into two groups where 64.3% of them fall between 20 and 30 years and remaining 35.7% were within 30–40 years of age [Figure 2].
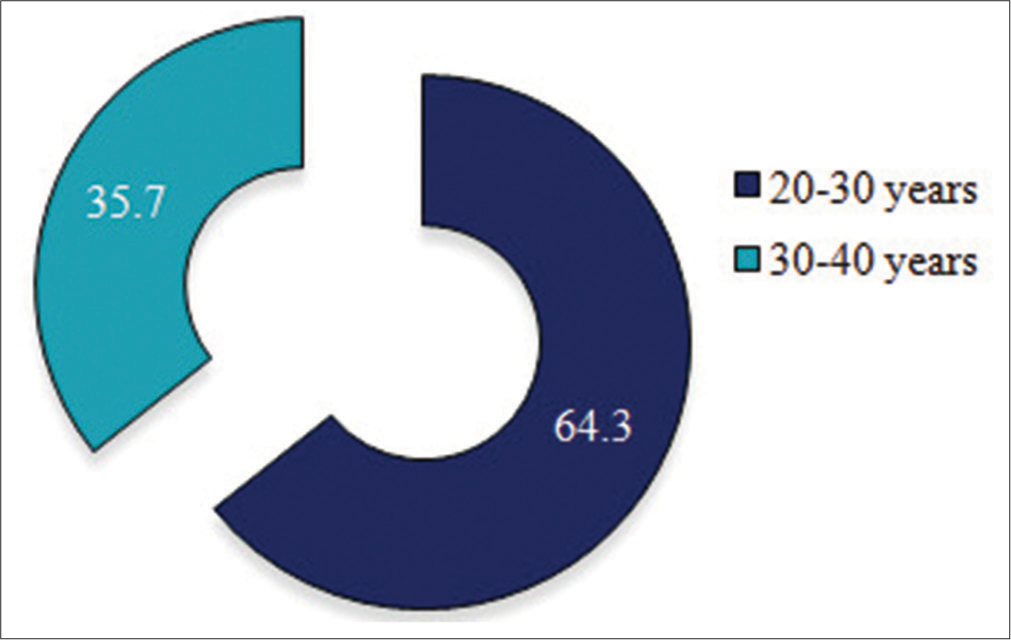
- Distribution of age groups among postpartum mothers.
Mode of delivery among postpartum mothers
About 60 patients underwent LSCS mode of delivery which adds up to a large portion of 85.7% compared to 14.3% who opted for NVD. While the cumulative percentage of patients in LSCS remains the same, it is increased to 100% in NVD [Table 1]. In the age group of 20–30 years, ~89% underwent LSCS and only 11% opted for NVD. However, of those within 30–40 years, 80% were referred for LSCS and relatively high percentage of patients (20%) preferred NVD than the lower age group [Table 2].
| Mode of delivery | ||||
|---|---|---|---|---|
| Mode of delivery | Frequency (n) | Percentage | Valid percentage | Cumulative percentage |
| LSCS | 60 | 85.7 | 85.7 | 85.7 |
| NVD | 10 | 14.3 | 14.3 | 100.0 |
| Total | 70 | 100.0 | 100.0 | |
LSCS: Lower segment cesarean section, NVD: Normal vaginal delivery
| Age | LSCS (%) | NVD (%) |
|---|---|---|
| 20–30 | 88.8 | 11.11 |
| 30–40 | 80 | 20 |
LSCS: Lower segment cesarean section, NVD: Normal vaginal delivery
Variation in Hb with age of postpartum patients
Between 20 and 30 years, Hb level varied from 7.9 to 15.2 g/dL with an average of 10.86 ± 1.49 g/dL. However, between 30 and 40 years, Hb level ranged from a minimum of 8.2 to a maximum of 12.4 g/dL with a mean value of 10.91 ± 1.52 g/dL [Table 3].
| Age | Hb levels (g/dL) (range) | Hb levels (g/dL) (mean value) |
|---|---|---|
| 20–30 | 7.9–15.2 | 10.86±1.49 |
| 30–40 | 8.2–12.4 | 10.91±1.52 |
Hb: Hemoglobin
Mode of delivery and Hb levels
Hb levels in LSCS varied from a very low value of 7.9 to a maximum of 15.2 g/dL with an average of 10.85 ± 1.42. In NVD patients, the range was relatively narrow with a minimum of 8.2 to a high of 12.4 g/dL with an average of 10.62 ± 1.27 [Table 4].
| Mode of delivery | Hb level (range) | Mean |
|---|---|---|
| LSCS | 7.9–15.2 | 10.85±1.42 |
| NVD | 8.2–12.4 | 10.62±1.27 |
LSCS: Lower segment cesarean section, NVD: Normal vaginal delivery, Hb: Hemoglobin
PPA
Among all postpartum mothers, about 54% showed moderate anemia (8–10.9 g/dL), followed by 24% mild (11–11.9 g/dL) and 2% with severe anemic (<8 g/dL) condition. Twenty percent of mothers after delivery had normal Hb content indicating healthy status [Figure 3]. The prevalence of anemia in the study population is ~56% comprising a significant proportion of the postpartum mothers. The number of PPA patients was higher in LSCS with 48 compared to NVD having 8. However, considering the total number of patients undergone LSCS (No: 60) and NVD (No: 10), the percentage of PPA and healthy individuals remains the same in both modes of delivery with 80% and 20%, respectively [Figure 4].
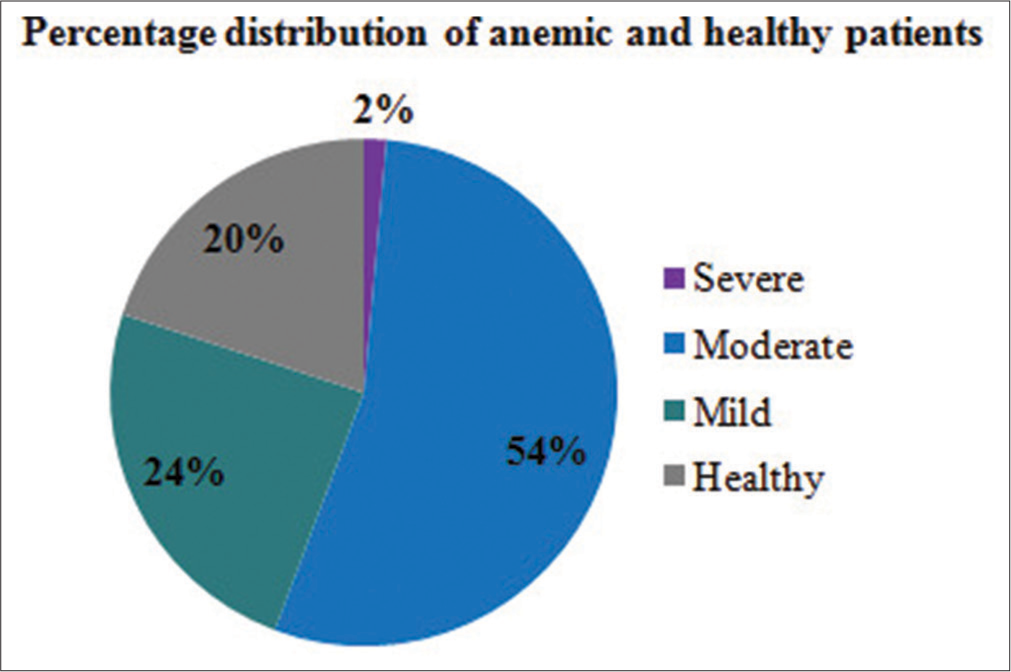
- Distribution of various stages of anemia among postpartum patients.

- Postpartum anemic and healthy patients in LSCS and NVD. LSCS: Lower segment cesarean section, NVD: Normal vaginal delivery.
Pearson correlation analysis
Pearson correlation analysis of Hb level with age and mode of delivery of postpartum mothers did not show any significant association (P > 0.05). However, a positive trend was observed between age and postpartum Hb level and a weak but negative correlation was observed with mode of delivery and Hb, especially with reference to NVD [Table 5].
| Correlation of age and Hb level | ||
| Age | Hb | |
| Age | ||
| Pearson correlation | 1 | 0.029 |
| P-value | 0.810 | |
| n | 70 | 70 |
| Correlation of mode of delivery and Hb level | ||
| Hb | Mode of delivery | |
| Hb | ||
| Pearson correlation | 1 | −0.058 |
| P-value | 0.632 | |
| n | 70 | 70 |
Hb: Hemoglobin, n: Number of samples
DISCUSSION
The alteration in Hb values during the postpartum period in an optimal antenatal care would be of greater significance as it can provide baseline information to prevent a lot of morbid complications. This study highlights PPA as a persistent yet unacknowledged cause of women morbidity. About 56% of individuals included in the study were anemic having moderate-to-severe anemia although the latter was only 2% [Figure 3]. The value of Hb in severe anemia was 7.9 g/dL and in moderate anemia, Hb ranged from 8.2 to 10.9 g/dL. An earlier study stated that PPA with Hb level <11 g/dL can affect 50% of women after 24–48 h of delivery.[9] A cross-sectional study on post-natal women from ethiopia reported 45% moderate anemia which is relatively less than the percentage obtained from our study (54%). However, these women had a high percentage (12%) of severe anemia as opposed to our findings.[10]
A study conducted at the primary health-care center in Tanzania showed 34.2% prevalence rate of PPA although the authors admit that the Hb kit used in the study may not mirror the present scenario.[2] Nevertheless, our study adds to the concern over high PPA in India as some previous studies also emphasized the prevalence of PPA of up to an alarming portion of 76.2% in the urban areas of Puducherry.[11] Similar percentage range (76.5%) of anemic patients was also recorded in a tertiary care teaching hospital at Mumbai in 2008 where severe anemia accounted about 10.3%.[12] Likewise, 70% anemia up to 6 weeks of postpartum period was reported among north Indian population.[13] Other crucial factors that lead to high rate of PPA in India include low iron reserve before and during pregnancy, poor socioeconomic background, pregnancy at younger age, narrow interval between births, and higher parity.[14] In contrast, studies from developed countries reported a general trend of lower prevalence of PPA. One of the states in Germany recorded an increase in PPA from 12.2 to 15.6% in the duration of 1998–2003. However, exceptionally, in the USA, anemia was diagnosed in 1 among every 5 cases of obstetric bleeding in the year 2003.[9] Globally, data from the year 2019 show that 39% of pregnant women suffered from anemia, and 50–80% of women from countries of poor and middle economic status had PPA.[15]
In our study, 85.7% underwent cesarean while 14.3% opted for vaginal delivery [Table 1]. This is contrary to the data from a hospital in Germany where 88% preferred vaginal delivery and 11.7% underwent cesarean.[9] Our data indicate that percentage of anemic patients is the same in LSCS and NVD mode with 80% each [Figure 4] suggesting more volume of blood loss as a possible reason in both cases, although we lack the prenatal Hb level for comparison. A study by obstetric department in a hospital in Germany including 43000 women at post-partum phase concluded that blood loss during delivery was the most important reason for PPA and it was especially high in LSCS.[9] As the rate of cesarean has increased significantly over the years, women undergoing LSCS are at a higher risk of PPA due to postpartum hemorrhage.[16] Hence, high iron intake during pregnancy should be facilitated.
There was no significant finding on variation of PPA in relation to age or mode of labor in our study. A study in Karnataka has shown the prevalence of PPA in mothers <20 years, especially in the case of <2-year interpregnancy interval. However, a significant difference with respect to age was not reported either.[17] Although there are a number of articles reporting the association of prenatal Hb level and mode of delivery, studies are scarce to support the relation between PPA and mode of delivery. Add to the existing data, our study showed an equal percentage of anemic patients in both modes of delivery.
Limitation of the study
Inclusion of pre-partum Hb levels, complete blood count, gravidity and parity information, body mass index, socioeconomic background, and expanding the sample size would be helpful to rule out specifically the underlying reasons for PPA in a community.
CONCLUSION
The present study highlights the prevalence of PPA associated with both LSCS and NVD mode of delivery and emphasizes on the importance of adequate measures to improve nutrition and health of women during pregnancy and postpartum period. PPA is considered an underestimated health concern; however, routine Hb estimation, consumption of iron-rich foods and iron and folic acid supplementation along with proper management of antenatal anemia, and regular follow-ups will be helpful to prevent PPA.
Acknowledgment
The authors are thankful to the MRD for assisting data collection.
Ethical approval
As this study is an audit of the clinical parameters, ethical approval is not mandatory.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
Dr. Sanjay Pasupathy is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Hemoglobin and hematocrit In: Walker HK, Hall WD, Hurst JW, eds. Clinical methods: The history, physical, and laboratory examinations (3rd ed). Boston, USA: Butterworth; 1990. Ch. 151
- [Google Scholar]
- Prevalence of post-partum anemia and associated factors among women attending public primary health care facilities: An institutional based cross-sectional study. PLoS One. 2022;17:e0263501.
- [CrossRef] [PubMed] [Google Scholar]
- Current concepts in postpartum anemia management. Curr Opin Anesthesiol. 2024;37:234-8.
- [CrossRef] [PubMed] [Google Scholar]
- Intravenous iron versus blood transfusion for postpartum anemia: A systematic review and meta-analysis. Syst Rev. 2024;13:9.
- [CrossRef] [PubMed] [Google Scholar]
- Physical health problems after childbirth and maternal depression at six to seven months postpartum. BJOG. 2000;107:1194-201.
- [CrossRef] [PubMed] [Google Scholar]
- Postpartum physical symptoms in new mothers: Their relationship to functional limitations and emotional well-being. Birth. 2008;35:179-87.
- [CrossRef] [PubMed] [Google Scholar]
- Listening to mothers: The first national US survey of women's childbearing experiences. J Obstet Gynecol Neonatal Nurs. 2002;31:633-4.
- [CrossRef] [PubMed] [Google Scholar]
- Physical symptoms after childbirth: Prevalence and associations with self-rated health. BJOG. 2005;112:210-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and risk factors for early postpartum anemia. Eur J Obstet Gynecol Reprod Biol. 2010;150:126-31.
- [CrossRef] [PubMed] [Google Scholar]
- Postpartum anemia and its determinant factors among postnatal women in two selected health institutes in Gondar, Northwest Ethiopia: A facility-based, cross-sectional study. Front Med (Lausanne). 2023;10:1105307.
- [CrossRef] [PubMed] [Google Scholar]
- High prevalence of anemia among postnatal mothers in Urban Puducherry: A community-based study. J Family Med Prim Care. 2019;8:2703-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of anemia in the postnatal women at a tertiary care teaching hospital in Mumbai. J Med Nutr Nutraceuticals. 2012;1:54-7.
- [CrossRef] [Google Scholar]
- Prevalence of anaemia in the postpartum period: A study of a North Indian village. Trop Doct. 2009;39:211-5.
- [CrossRef] [PubMed] [Google Scholar]
- Federation of obstetric and gynecological societies of India consensus recommendations for the management of postpartum anemia with specific reference to usage of ferric carboxymaltose. J South Asian Fed Obstet Gynecol. 2024;16:S44-9.
- [CrossRef] [Google Scholar]
- A rapid landscape review of postpartum anaemia measurement: Challenges and opportunities. BMC Public Health. 2023;23:1454.
- [CrossRef] [PubMed] [Google Scholar]
- A study of maternal morbidity associated with caesarean delivery in tertiary care hospital. Int J Community Med Public Health. 2017;4:1542-7.
- [CrossRef] [Google Scholar]
- Prevalence of anaemia among postnatal mothers in coastal Karnataka. J Clin Diagn Res. 2016;10:LC17-20.
- [CrossRef] [PubMed] [Google Scholar]







