Translate this page into:
A case report on the comprehensive management of recurrent fractures in polyostotic Paget’s disease

*Corresponding author: S. Chandru, Department of Pharmacy Practice, Ganga Medical Centre and Hospital, Coimbatore, Tamil Nadu, India. dr.chandrusasikumar3114@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chandru S, Ahamed SMM, Kumar RP, Duraisingh LB, Kenslin P. A case report on the comprehensive management of recurrent fractures in polyostotic Paget’s disease. Glob J Health Sci Res. doi: 10.25259/GJHSR_40_2024
Abstract
Paget’s disease of the bone is a chronic and long-lasting disorder that causes bones to grow larger and become weaker than normal. Pelvis, skull, spine, and leg bones are the most commonly affected bones and Paget’s disease affects just one or a few bones from the skeletal system. This metabolic bone disease does not come with specific symptoms and the people affected are found with no symptoms in some scenarios. However, bone changes occur which can result in ostealgia or osteodynia, malformed and fragile bones prone to recurrent fractures, tumors, inflammation, and arthritis in the joints close to the affected bones. At times, Paget’s illness is discovered by incident during a routine X-ray or blood test. The symptoms can be managed with surgical interventions and medications which improve pain and control the effects of the disease. The exact factor causing the condition is unknown but some factors contributing may include genetic, lifestyle factors, such as poor diet, or bone injury in early life which may trigger the development of Paget’s disease. Our case report explicates about a 70-year-old male patient who had an alleged history of slip and fall at home and sustained an injury to the right thigh and leg. The patient was a known case of Paget’s disease who underwent dynamic hip screw fixation surgery for right femur in the former hospital admission. This case report elaborates on the medical management with calcium and vitamin supplements along with bone modifying agents and surgical intervention proceeded in the recurrent fractures with the underlying mechanism of the illness.
Keywords
Paget’s, fractures
Surgical intervention
Medical management physiotherapy
Nursing care
INTRODUCTION
Sir James Paget initially endorsed osteitis deformans, often referred to as Paget’s disease of bone (PDB), over two centuries a while ago.[1] PDB can present as either monostotic or polyostotic, with the former being more common and typically affecting the axial skeleton. The disease can impact all bones of the craniofacial complex to varying extents.[2] It is characterized by focal alterations in bone remodeling, leading to bones with abnormal structure and mechanical properties, often associated with pain and pathological fractures.[3] Paget’s disease progresses through four distinct phases: Primary osteoclastic activity (osteolytic) combines osteoclastic and osteoblastic activity (mixed), primary osteoblastic activity (osteosclerotic), and rarely, malignant transformation. Complications include fractures, bone deformities, secondary osteoarthritis, neurological issues such as nerve compression, cranial involvement causing deafness and vertigo, and the development of sarcomas, such as osteosarcoma.[4]
CASE REPORT
A 70-year-old male patient was alleged to have a history of slips and falls at home and sustained injuries to the right thigh and leg. The patient has complained of pain over the right thigh and left leg, and he has been unable to bear weight or walk since the injury. There was no history of loss of consciousness, vomiting, seizures, or ENT bleeding. The patient went to a nearby hospital where an X-ray was taken, first aid was done, and then, he came to the Ganga hospital for further treatment. The patient has already been diagnosed with Paget’s disease. In December 2023, he underwent dynamic hip screw (DHS) fixation surgery for the right femur for a subtrochanteric femur fracture. He has co-morbidities such as diabetes mellitus and hypertension and is on regular medications which include tablet glycomet 500 mg 1-0-1 and tablet hipres 50 1-0-0. General examinations are normal. Local examination of the left knee reveals swelling and soreness over the knee; knee range of motion (ROM) cannot be accessible due to pain; active toe extension and flexion are present; the dorsalis pedis and posterior tibial pulse are palpable; and sensation is intact. Local examination of the right knee reveals soreness over the middle third femur; knee ROM cannot be accessible due to pain; active toe extension and flexion are present; the dorsalis pedis and posterior tibial pulse are palpable; and sensation is intact. Laboratory investigations for Paget’s disease are shown in Table 1.
| Test name | Result | Unit | Range |
|---|---|---|---|
| Beta-cross laps | 825.2 | pg/mL | Age men (95% pg/mL) <29.9 |
| N-MID Osteocalcin | 21.49 | ng/mL | Healthy women premenopausal/>20 |
| Serum alkaline phosphatase | 18.9 | ng/mL | <20 ng/mL deficiency 21–30 ng/mL insufficiency |
| HbA1c | 7.1 | % | <6% normal |
HbA1c: Hemoglobin A1c, N-MID Osteocalcin: N-terminal/midregion osteocalcin
Both legs are swollen on the inner sides. A Doppler ultrasound of the veins in both lower limbs was performed, and the results showed no indication of deep vein thrombosis. X-ray imaging of the right hip with the femur in AP/lateral views indicated the presence of a peri-implant located in the middle third of the femur shaft, alongside a non-united subtrochanteric femur fracture with a DHS in situ. The X-ray of the left leg in anterior-posterior (AP)/lateral view indicated a fracture in the middle portion of the tibia shaft with visible bowing. A pelvic X-ray in AP view illustrated sclerosis, notably along the iliopubic sign and ischial illness, as well as coarsening of the trabecular pattern and thickening of the pelvic brim, often referred to as the “Brim sign,” as shown in Figure 1. In addition, a fluorodeoxyglucose (FDG) computed tomography (CT) positron emission tomography (PET) can indicate abundant bone expansion with cortical thickening and coarsening of trabeculae in the right femur, along with the presence of a fracture as described, suggesting the likelihood of polyostotic Paget’s disease with pathological features, as shown in Figure 2.
As Paget’s disease involves the heart, the cardiologist reviewed the patient’s medical history, noting hypertension and diabetes mellitus. Both the electrocardiogram and echocardiogram results were within normal limits. The diabetologist conducted laboratory investigations for type 2 diabetes mellitus, with the results provided in Table 1. The geriatrician and general medicine specialist diagnosed the patient with Paget’s recurrent fractures. He recommended vitamin D and calcium and initiating bisphosphonate therapy following surgery. Following the complex surgical interventions, including implant removal, biopsy, and extensive orthopedic procedures such as open reduction internal fixation (ORIF) with antegrade femoral nailing (AFN) nailing for the right femur and corrective osteotomy, along with closed reduction internal fixation (CRIF) using suprapatellar nailing for the left tibia, the post-operative care plan was specific to address the patient’s needs. Upon discharge, the patient received an intravenous infusion of zoledronic acid at a rate of 5 mg/100 mL over 15 min, along with a single dose of 100 mg IV hydrocortisone and a 50 mg IM Avil administered immediately. Subsequently, 1 g of tamin was given right after the zoledronic acid infusion. A comprehensive follow-up appointment was scheduled to monitor the patient’s alkaline phosphatase level after 3 months. If the alkaline phosphatase level decreases, the patient will continue the yearly zoledronic acid treatment. If the alkaline phosphatase level increases, zoledronic acid treatment will be initiated every 3 months. Further, the patient was instructed to take a daily regimen of calcitonin nasal spray for its benefits in regulating bone metabolism. In addition, calcium and vitamin D supplements continued to enhance bone health and help in the healing process.

- Brim Sign.
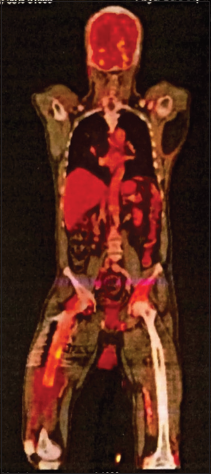
- Features of polyostotic Paget’s disease.
DISCUSSION
PDB, identified by Dr. James Paget in 1877, is characterized by disorganized bone remodeling, resulting in abnormal bone architecture, increased fragility, and a predisposition to fractures. Despite extensive research, the exact etiology remains unclear, with genetic mutations (e.g., the SQSTM1 gene), viral infections (paramyxovirus), and metabolic disturbances being potential contributors. The disease progresses through four phases: osteolytic, mixed osteoclastic-osteoblastic, osteosclerotic, and rarely malignant transformations.[1,3,5]
The presented case involves a 70-year-old male with recurrent fractures, a common and debilitating complication of advanced Paget’s disease. Patient management was complicated by comorbidities, including diabetes mellitus and hypertension. Clinically, he exhibited significant pain, impaired mobility, and localized tenderness in the affected area, typical of Paget’s disease.
Effective management of Paget’s disease, particularly with recurrent fractures, necessitates a multidisciplinary approach. Pharmacological treatment with bisphosphonates, notably zoledronic acid, is crucial in reducing bone turnover and preventing further fractures. In this case, zoledronic acid is given postoperatively for optimal therapeutic effect.[6-9] In addition, calcitonin nasal spray was recommended to help regulate bone metabolism.[10] Vitamin D, along with calcium medication, plays a vital role in bone health and healing, and the patient’s diet should include vitamin D and calcium-rich foods to improve bone health.[11,12]
Surgical intervention is frequently necessary to fix fractures and repair abnormalities. The patient underwent various orthopedic procedures, including implant removal, biopsy, ORIF with AFN for the right femur, and CRIF with suprapatellar nailing for the left tibia. Post-operative care focuses on pain management, infection prevention, and rehabilitation to regain function and mobility.
Physiotherapy was essential in the patient’s rehabilitation process, helping to restore function and mobility. Tailored physiotherapy programs focus on improving strength, flexibility, and overall function, which are critical for recovery in patients with Paget’s disease.
Nurses played an essential role in the comprehensive care of this patient. They were responsible for providing drugs, monitoring vital signs, treating pain, avoiding infection, and providing education on lifestyle modifications to support bone health. Nurses also helped the patient and the multidisciplinary team communicates better, resulting in a more coordinated approach to care.
The diagnosis was confirmed by a laboratory test that showed a high level of serum alkaline phosphatase and a normal level of calcium, which is in line with the biochemical profile of Paget’s disease.[13] Imaging methods, such as X-rays and FDG CT PET scans, were useful in assessing the disease’s extent and activity, displaying typical signs such as bone bowing, cortex thickening, and the “Brim sign.” Regular follow-up and monitoring of serum alkaline phosphatase levels were necessary to assess therapy response and adjust the therapeutic strategy as needed.
CONCLUSION
This case highlights the complexity of managing advanced PDB, particularly in elderly patients with comorbidities. The successful treatment of recurrent fractures in this patient required a comprehensive multidisciplinary approach. Pharmacological therapy with bisphosphonates and calcitonin effectively reduces bone turnover and supports bone health. Surgical interventions were crucial for stabilizing fractures and correcting deformities, while postoperative care, including physiotherapy, was essential for restoring function and mobility. Nurses played a key role in the patient’s recovery by administering medications, managing pain, preventing infection, and providing education on lifestyle modifications. Regular follow-up and monitoring of biochemical markers were vital in assessing treatment response and guiding future therapeutic decisions. This case underscores the importance of a coordinated and holistic approach in managing complex cases of PDB.
Acknowledgment
The authors would like to express their sincere gratitude to the medical, nursing, and support staff for their invaluable contributions to the patient’s care and management. Special thanks are also extended to the colleagues and peers who provided critical insights and suggestions that greatly enhanced the quality of this case report. We appreciate the patient’s cooperation and consent, which made this publication possible.
Ethical approval
Institutional Review Board approval is not required.
Declaration of the patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- On a form of chronic inflammation of bones (osteitis deformans) Med Chir Trans. 1877;60:37-649.
- [CrossRef] [PubMed] [Google Scholar]
- Paget disease of bone: A classic case report. Contemp Clin Dent. 2013;4:227-30.
- [CrossRef] [PubMed] [Google Scholar]
- Benign fibro-osseous lesions of the craniofacial complex a review. Head Neck Pathol. 2008;2:177-202.
- [CrossRef] [PubMed] [Google Scholar]
- Histology, osteoclasts In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023.
- [Google Scholar]
- Failure to detect measles virus ribonucleic acid in bone cells from patients with Paget's disease. J Clin Endocrinol Metab. 2008;93:1398-401.
- [CrossRef] [PubMed] [Google Scholar]
- Use of zoledronic acid in the treatment of Paget's disease. Ther Clin Risk Manag. 2007;3:913-8.
- [Google Scholar]
- Single infusion of zoledronate in Paget's disease of bone: A placebo-controlled, dose-ranging study. Bone. 1999;24:81-S-5.
- [CrossRef] [PubMed] [Google Scholar]
- Zoledronate treatment in active Paget's disease. Ann Rheum Dis. 2003;62:275-6.
- [CrossRef] [PubMed] [Google Scholar]
- Emerging strategies and therapies for treatment of Paget's disease of bone. Drug Des Devel Ther. 2011;5:225-39.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Paget's disease with the calcitonins. Aust N Z J Med. 1979;9:36-43.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D status in paget disease of bone and efficacy-safety profile of cholecalciferol treatment in pagetic patients with hypovitaminosis D. Calcif Tissue Int. 2019;105:412-22.
- [CrossRef] [PubMed] [Google Scholar]
- Paget's disease of bone and calcium homeostasis: Focus on bisphosphonate treatment. Exp Clin Endocrinol Diabetes. 2011;119:519-24.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of Paget's disease of bone. Clin Invest Med. 2007;30:E210-23.
- [CrossRef] [PubMed] [Google Scholar]







