Translate this page into:
Balancing risks and outcomes in schwannoma treatment: Case series

*Corresponding author: Kumar Saket, Department of Oral and Maxillofacial Surgery, Rajiv Gandhi University of Health Sciences, Bengaluru, Karnataka, India. saket0410@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saket K, Mahableshwara CH, Kumar DP, Sutradhar D. Balancing risks and outcomes in schwannoma treatment: Case series. Glob J Health Sci Res. doi: 10.25259/GJHSR_27_2024
Abstract
Schwannomas are rare benign tumors originating from Schwann cells of peripheral nerve sheaths, occasionally presenting intraosseously in the oral and maxillofacial region. Management decisions for these tumors require careful consideration of their location, size, and impact on surrounding structures. We present two contrasting cases of schwannomas: One involving a non-surgical approach due to extensive involvement and proximity to critical structures and the other necessitating surgical excision for a well-defined intraosseous lesion. The first case, in a 28-year-old female, highlighted the decision to monitor the lesion due to its significant size and location, while the second case, in a 20-year-old female, demonstrated successful surgical removal with histopathological confirmation of a benign schwannoma. These cases underscore the importance of tailored management strategies based on thorough clinical, radiographic, and histopathological assessments to optimize outcomes and minimize risks associated with surgical intervention.
Keywords
Schwannoma
Maxilla
Benign tumor
Masticatory space
Intraosseous
INTRODUCTION
Schwannomas, also known as neurilemmomas, are benign tumors that arise from Schwann cells of the peripheral nerve sheath. Although schwannomas can occur throughout the body, their presence in the oral and maxillofacial region is relatively rare, particularly as intraosseous lesions. These tumors are typically slow-growing and often asymptomatic, which can pose a diagnostic challenge and influence management strategies.[1]
The management of schwannomas requires a careful assessment of the lesion’s characteristics, location, and potential impact on surrounding anatomical structures. Surgical excision is generally the preferred treatment for schwannomas due to their benign nature and encapsulated growth pattern, which typically allows for complete removal with low recurrence rates. However, the decision to operate must consider the potential risks, especially when lesions are located near critical anatomical structures.[2]
This article presents two contrasting cases of schwannomas in the oral and maxillofacial regions and highlights the importance of individualized management approaches based on comprehensive clinical, radiographic, and histopathological evaluations.[3]
CASE SERIES
Case 1: Schwannoma in the left masticatory region
A 28-year-old female presented with a history of minimal erosion on the left buccal mucosa and reported a painless, solitary, non-tender, non-pulsatile, and firm mass in the left masticatory region, persisting for 1 year. Her medical history was unremarkable, and there was no history of trauma at the site. Clinical examination revealed a non-tender, firm mass measuring 3.5 cm × 3 cm. Cranial nerve examination was normal, and there was no hindrance in muscle movements, numbness, or weakness [Figure 1].
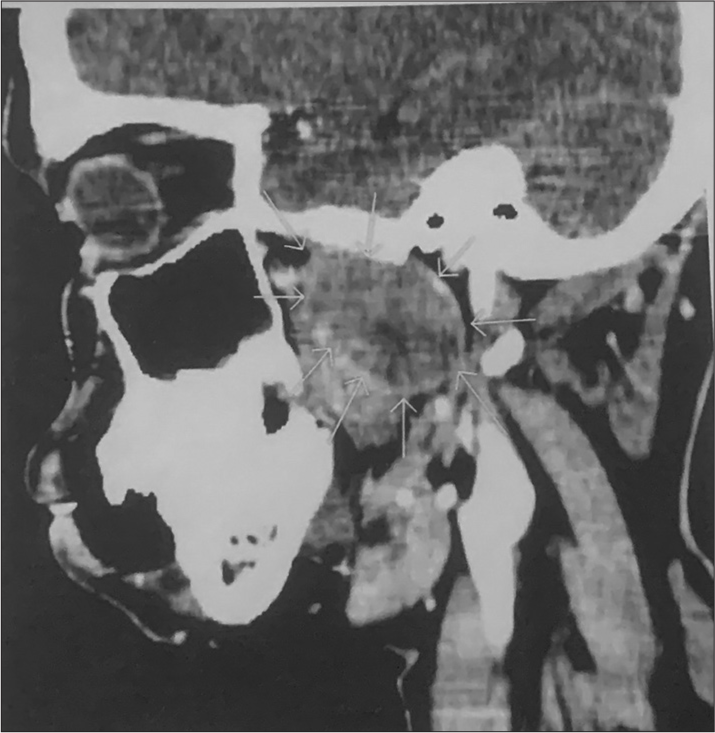
- A 28-year-old female contrast-enhanced computed tomography sagittal view arrows showing 3.5 × 3 cm mass in left masticatory space.
Fine-needle aspiration cytology (FNAC) was non-diagnostic. Contrast-enhanced computed tomography (CT) revealed a non-homogeneous, isodense mass measuring 3.5 cm × 3 cm in the left masticatory space, projecting toward the left side of the oropharynx, and displacing the parapharyngeal fat. The mass extended superiorly to the level of the skull base without erosion and laterally up to the neck of the left condyle of the mandible. In addition, a few small lymph nodes measuring approximately 12 mm were identified in the left level IB region. Magnetic resonance imaging (MRI) was not performed due to financial constraints.
The imaging characteristics suggested a schwannoma [Figure 2]. Given the lesion’s extensive involvement and critical location near the skull base and mandible, surgery was deemed high risk. Potential surgical complications included significant functional impairment, risk of nerve damage, and potential for incomplete resection due to the complex anatomy and proximity to vital structures. The patient’s cranial nerve function and muscle movements were unaffected, indicating a low impact on her current quality of life. Therefore, a decision was made to avoid surgical intervention and instead consider non-invasive monitoring.
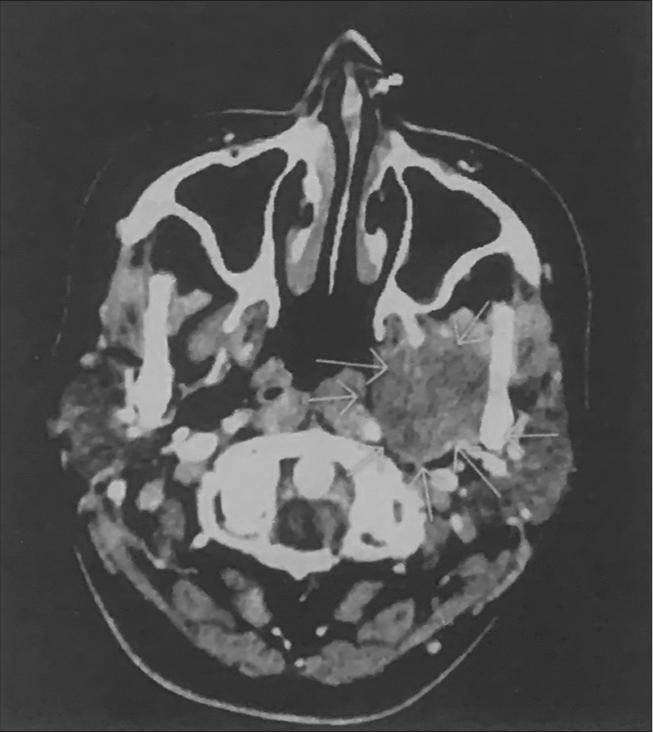
- Computed tomography axial view revealed a mass measuring 3.5 cm × 3 cm arrows showing left side oropharynx mass.
This non-surgical approach was justified as the mass exhibited benign characteristics, non-homogeneous enhancement, and isodense features, reducing the urgency for immediate removal. Regular follow-up was planned to monitor any changes in the lesion’s behavior. In addition, radiotherapy was considered a potential treatment option to control the tumor’s growth and manage symptoms if necessary.
A 1-year follow-up showed no significant change in the size or characteristics of the mass, and the patient remained asymptomatic with normal cranial nerve function and muscle movements. Regular consultations with an oncologist specializing in radiotherapy continued to evaluate the appropriateness and timing of this treatment approach.
Case 2: Intraosseous schwannoma of the maxilla
A 20-year-old female was referred to the Department of Oral Medicine, Diagnosis, and Radiology at KVG Dental College and Hospital, Sullia, for a detailed intraoral examination after a private dental practitioner detected a periapical lesion during a routine radiograph for proximal caries diagnosis. The patient was asymptomatic with an unremarkable medical and dental history.
Clinical examination revealed an ill-defined, solitary swelling of approximately 1 cm × 3 cm in the left lateral part of the anterior hard palate near the lateral incisor and canine [Figure 3]. The swelling was non-tender and bony hard on palpation, with no fluctuation or softening. The patient had no history of trauma, and the maxillary anterior teeth responded positively to electric and thermal pulp vitality tests, eliminating the possibility of a periapical cyst or odontogenic cyst.
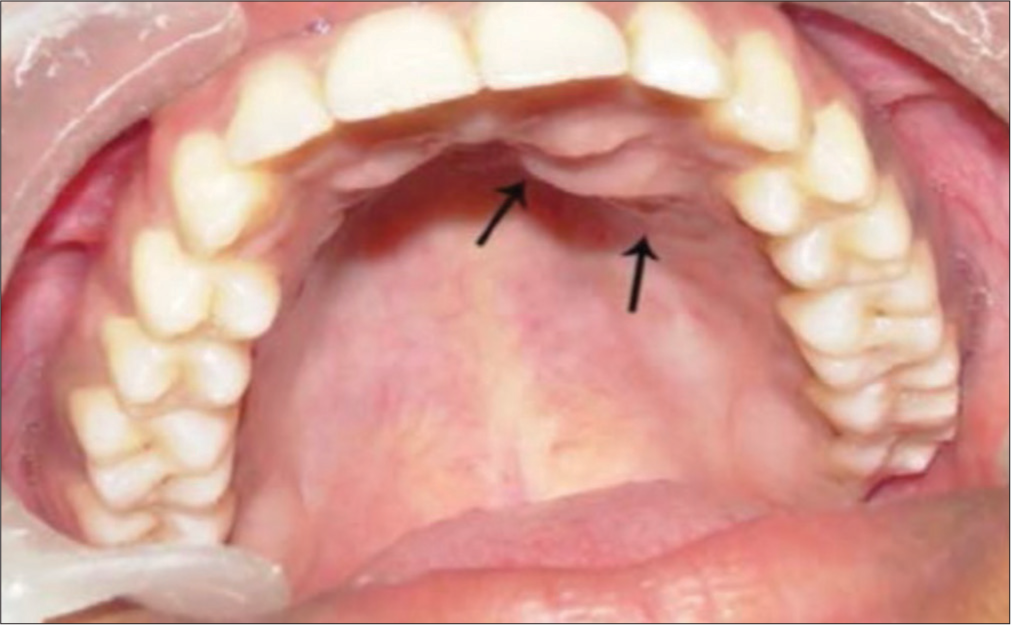
- Anterior hard palate showing an ill-defined swelling in the left lateral incisor-canine region arrows showing 1 × 3 cms mass.
Radiographic examination showed a well-defined radiolucent lesion approximately 2 mm × 3 mm with an interrupted corticated border at the root apices of the canine and first premolar [Figure 4]. A maxillary lateral occlusal radiograph revealed a well-defined unilocular radiolucent lesion (2 mm × 3 mm) overlapping the roots of the lateral incisor, canine, and first premolar, lined by irregular cortical margins. Aspiration biopsy was negative for cystic fluid or blood, suggesting an odontogenic or non-odontogenic intraosseous tumor.
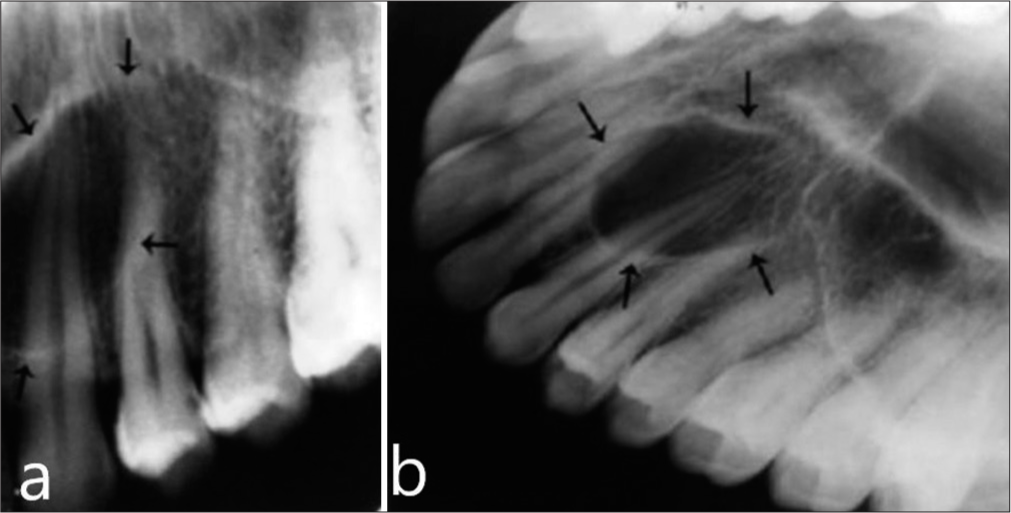
- Intraoral periapical radiograph of maxillary left canine region (a) well circumscribed unilocular oval radiolucent lesion with interrupted cortical margins, first arrow showing extension from upper border to the second arrow superimposing over the root spices. (b) Arrows marking on Maxillary occlusal radiograph demonstrating unilocular radiolucent lesion extending from the left lateral incisor to first premolar, overlapping on their roots.
Given the lesion’s well-defined and encapsulated nature, surgical excision was performed under local anesthesia. The lesion was easily separated from the surrounding healthy bone due to its encapsulation within dense fibrous connective tissue [Figure 5]. The surgical defect was closed with sutures, and an acrylic removable partial denture (stent) was fabricated to cover the dressing area to prevent infection and facilitate wound healing.

- Surgical exposure revealing a well-encapsulated, unilocular lesion situated in the left lateral incisor-canine region.
Histopathological examination of the excised specimen revealed a tumor mass composed of neural tissue with Antoni type A and Antoni type B patterns. The presence of spindle-shaped cells arranged in a palisading pattern forming Verocay bodies and microcyst formation confirmed the diagnosis of benign schwannoma. No cellular atypia or malignancy was observed [Figure 6].
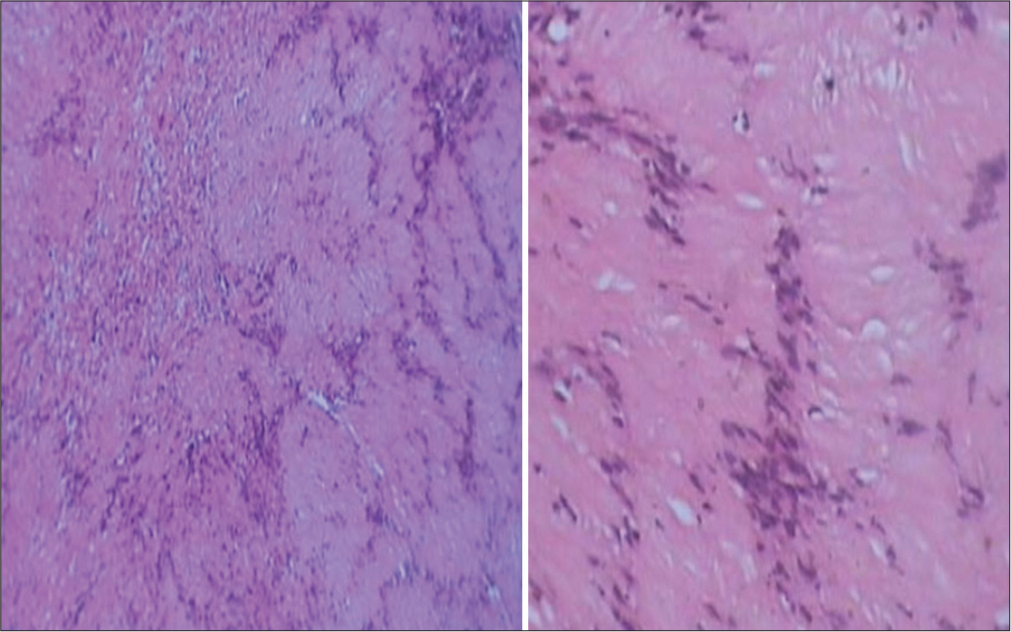
- Photomicrograph of the lesion showing Antoni B tissue. Photomicrograph of the lesion composed of densely cellular and irregularly arranged, elongated spindle cells with palisading nuclei and Verocay bodies. Numerous blood vessels are seen interspersed throughout the histopath imaging.
Post-operative follow-up after 2 months showed remarkable soft-tissue healing, although the underlying bone remained soft due to the bony defect. A 2-year radiographic evaluation revealed complete bone regeneration with no signs of recurrence [Figure 7]. A general physical examination ruled out multiple tumours of neural origin in other sites.
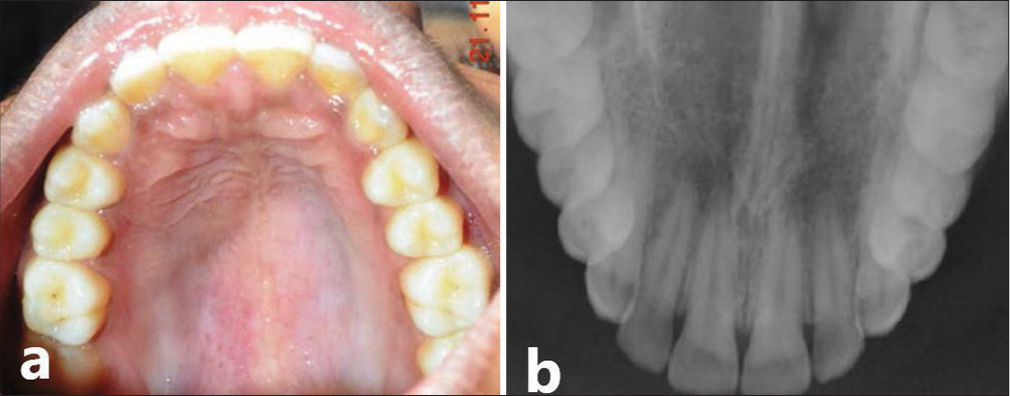
- Two year post operative. (a) Clinical view of Maxilla. (b) Maxillary occlusal radiograph demonstrating palate with a normal trabecular pattern at the operated site indicating complete bone formation.
DISCUSSION
Schwannomas, also known as neurilemmomas, are rare, benign, encapsulated nerve sheath tumors of unknown etiology. The management of schwannomas requires careful consideration of the lesion’s characteristics, location, and potential impact on surrounding structures. This discussion highlights key points from the literature to elucidate when surgical intervention is warranted and when conservative management might be preferable.
Surgical excision is typically recommended for schwannomas due to their benign nature and encapsulated growth, which usually allows for complete removal with low recurrence rates. As noted by Chrysomali et al.,[1] surgical intervention is crucial when the tumor presents with significant clinical symptoms, rapid growth, or compression of adjacent structures. Similarly, the decision to operate on intraosseous schwannomas is often based on the risk of bone destruction and potential impact on dental structures, as seen in our second case, where the lesion was localized and well-defined, making it amenable to complete surgical removal with favorable outcomes.[1] A case report by Enzinger and Weiss describes a 36-year-old female with a slow-growing, painless schwannoma on the hard palate, which was surgically excised and confirmed through histopathology. No recurrence was observed postoperatively, and the prognosis was favorable. Similarly, Koopaie et al.[2] reported a 13-year-old boy with a painless, slow-growing schwannoma on the hard palate, which was surgically excised and confirmed histopathologically, with no recurrence observed postoperatively.
Conversely, the decision to avoid surgery may be justified in cases where the schwannoma is situated in a high-risk location or involves extensive anatomical structures, making surgical excision risky. This was the approach in our first case, where the lesion in the left masticatory region was deemed too risky to operate due to its proximity to the base of the skull and the potential involvement of critical neurovascular structures. Iwamoto and Fine emphasize that conservative management, including regular monitoring and imaging, is appropriate for asymptomatic schwannomas or those in challenging locations where surgical morbidity would outweigh the benefits.[3] Similarly, a case report by Siddig et al.[4] reported a 55-year-old female with a non-tender, firm intraoral schwannoma in the soft palate, where conservative management was chosen due to potential surgical risks and non-diagnostic FNAC.
The diagnostic process for schwannomas involves a combination of clinical examination, radiographic imaging, and histopathological analysis. Schwannomas can often be mistaken for other types of lesions due to their non-specific presentation. FNAC and imaging techniques such as CT and MRI are valuable in differentiating schwannomas from other potential diagnoses, as highlighted by Khaleque et al. In our second case, detailed radiographic evaluation and histopathological examination confirmed the diagnosis, guiding the successful surgical intervention.[5] Histopathologically, schwannomas exhibit characteristic Antoni A and Antoni B tissue patterns. Antoni A tissue consists of densely packed cells with palisading nuclei and Verocay bodies, whereas Antoni B tissue is less organized with a more myxoid appearance. These features are critical for definitive diagnosis, as seen in both of our cases, where histopathological analysis confirmed the benign nature of the tumors.
If a schwannoma is left untreated, it may grow slowly and remain asymptomatic for a long time, especially in noncritical areas. However, as it enlarges, it can cause symptoms due to pressure on adjacent tissues and, although rare, may undergo malignant transformation into a malignant peripheral nerve sheath tumor (MPNST). According to a study by Evans DG et al.,[6] radiotherapy has shown promising results in controlling the growth of benign schwannomas, providing an effective non-surgical option for patients. An illustrative case in the literature involves a patient with a large trigeminal schwannoma where surgery was deemed high-risk due to its location near critical structures. The patient underwent fractionated stereotactic radiotherapy, resulting in significant tumor shrinkage and symptom improvement without major complications.
Clinical presentation and diagnostic evaluation
Schwannomas typically manifest as slow-growing, painless masses that may become symptomatic as they enlarge and exert pressure on adjacent tissues. Diagnostic evaluation involves a combination of clinical examination, radiographic imaging, and histopathological analysis. FNAC, alongside imaging modalities such as CT and MRI, play pivotal roles in confirming the diagnosis and assessing tumor extent.
Histopathologically, schwannomas exhibit distinct tissue patterns, including Antoni A (dense, palisading cells with Verocay bodies) and Antoni B (less organized, myxoid appearance), crucial for definitive diagnosis and differentiation from other lesions.
Indications for surgical intervention
Surgical excision remains the cornerstone of treatment for schwannomas, primarily due to their benign nature and encapsulated growth, which typically allows for complete removal with low recurrence rates. The decision for surgery is guided by several factors:
Symptomatic presentation
Schwannomas causing significant clinical symptoms or neurological deficits often necessitate surgical intervention to relieve pressure on adjacent structures and prevent functional impairment.
Rapid growth or compression
Tumors demonstrating rapid growth or compression of vital structures, as highlighted by Hilton DA et al.,[7] require prompt surgical management to mitigate potential complications.
Anatomical considerations
Lesions in critical anatomical locations, such as near neurovascular bundles or within bone structures, pose challenges for surgery and may necessitate alternative approaches or conservative management.
Conservative management approaches
In cases where surgical excision is deemed high-risk or potentially morbid, conservative management strategies are considered. This approach includes regular monitoring with imaging studies to assess tumor growth and symptom progression, as advocated by Iwamoto and Fine. Conservative management is particularly justified for asymptomatic schwannomas or those located in challenging anatomical sites where the risks of surgery outweigh the benefits.
Alternative therapeutic options
Radiotherapy, specifically fractionated stereotactic radiotherapy, has emerged as a promising non-surgical option for controlling the growth of benign schwannomas, particularly in inoperable cases or those where surgery poses significant risks. Studies in literature and illustrative cases highlight successful outcomes with radiotherapy in reducing tumor size and improving symptoms without major complications.
Long-term prognosis and considerations
Untreated schwannomas can remain asymptomatic for extended periods but may lead to symptoms as they enlarge. Rarely is there a risk of malignant transformation into MPNST, underscoring the importance of monitoring and timely intervention.
CONCLUSION
The management of schwannomas in the oral and maxillofacial region must be individualized, taking into account the lesion’s size, location, symptomatology, and potential risks associated with surgical intervention. While surgical excision remains the mainstay of treatment for accessible and symptomatic schwannomas, conservative management is a viable option for lesions in high-risk areas or those presenting with minimal symptoms. Comprehensive clinical, radiographic, and histopathological evaluations are essential in guiding appropriate management strategies to ensure optimal patient outcomes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Peripheral odontogenic fibroma: Report of a case and review of the literature. J Oral Maxillofac Surg. 1997;55:292-5.
- [Google Scholar]
- Schwannoma of the hard palate in a child: Case report. Arch Mil Med. 2019;7:e98076.
- [CrossRef] [Google Scholar]
- Schwannoma of the maxillary sinus: Case report and review of the literature. Neurosurgery. 2000;46:479-82.
- [Google Scholar]
- Uncommon finding of a soft palate schwannoma: A case report. Cureus. 2023;15:e50172.
- [CrossRef] [Google Scholar]
- Intraosseous schwannoma of the mandible: A case report. J Oral Maxillofac Sura. 2018;76:233-8.
- [Google Scholar]
- Radiation treatment of benign tumors in NF2-related schwannomatosis: A national study of 266 irradiated patients showing a significant increase in malignancy/malignant progression. Neurooncol Adv. 2023;5:vdad025.
- [Google Scholar]







